The year was 1978. I was a newly married, 25-year-old registered nurse working on a medical unit at Mercy Medical Center in Oshkosh, Wis. I began to notice morning stiffness, increasing fatigue, and bilateral heel and ankle pain. Every step hurt as I walked down the halls to care for my patients. My diagnosis was early rheumatoid arthritis (RA), confirmed by blood work.
I began a daily regimen of 13 enteric-coated aspirin a day, which did nothing to help the pain and stiffness I felt. In the next 40 years, my RA would force me to undergo 14 orthopedic surgeries, give myself daily and weekly injections, swallow thousands of pills and become the patient of an array of healthcare providers. As I look back on those 40 years, I am thankful that I was able to live a fulfilling life as a wife, mother, grandmother, nurse and friend. Many people were placed into my life at just the right time to give me the right treatment, counseling and support I so desperately needed. I want to introduce some of them to you. And alert you to some of the lessons I’ve learned over the years.
Don’t Miss the Fun Stuff
The foundation of an RA patient’s care should be a rheumatologist. I have been the patient of five rheumatologists during the course of my arthritis. Jeanna Owens, MD, was the second one who cared for me while I lived in Wisconsin. She was a very wise doctor.
In 1990, my family planned a trip to Walt Disney World. Shortly before we were to leave, my symptoms began to flare. I told Dr. Owens that I had decided not to go along to Florida. She looked at me, raised her eyebrows and firmly said, “Oh yes, you’re going. I want you to rent a wheelchair and ride in it. You will save energy and can still go along.”
I took her advice. Our family was able to do everything we wanted and because I was in a wheelchair, we were escorted to the front of every line. My daughter, Laura, remarked, “Boy, this is great, Mom! That’s one good thing about your arthritis. We get to be first in line.”
Ask for Help
One of the hallmarks of a good rheumatologist is the ability to observe, analyze and uncover the often-subtle symptoms of RA that may go undetected for years. It takes time to completely review a patient’s extensive history to determine the optimum treatment for that patient. Eric Gowing, MD, was able to do that for me while I still lived in Wisconsin. After pouring over my history, he saw red flags, which he clearly explained.
Dr. Gowing always encouraged me to ask questions and never edged his way to the door of the exam room until I had my answers. He once told me, “Having RA is very humbling. You have to swallow your pride and ask for help.” He was absolutely right. I still struggle with asking for help even after 40 years.

Sarah Troxell and Eric Gowing, MD.

Sarah Troxell and Heidi Schneider, MD.

Richard Moore, MD, and Sarah Troxell.

Sarah Troxell and David Romond, MD.
Communication Is Key
Several years ago I became the patient of Heidi Schneider, MD, in Tyler, Texas. Her rheumatology practice offers a patient portal, called MyChart, which includes the option to “communicate with your doctor.” I have been able to ask a question or report a new development to her, and she usually answers me on the same day. I don’t know how she finds the time to do this, but she does. She is one of the most caring and approachable doctors I have ever known.
My History
Hips: My long-standing RA has seriously damaged my joints, forcing me to have 14 orthopedic surgeries. My trips to the operating room included bilateral hip arthroplasties done in 1994 at age 41. My arthroplasties served me well until 2005, when I noticed a new pain in the iliotibial band area of my right leg. I went to see my orthopedic surgeon, David Romond, MD, of Oshkosh, Wis., who had done my arthroplasties.
He always did his best to communicate what type of surgery he wanted to do, using anything available. Often, he used a 4×4 package, and on it he drew a picture of what he planned to do. After my hip was X-rayed, Dr. Romond showed me the result and, with a very troubled look on his face, said, “Sarah, you need a revision.”
“A what?” I gasped. I had never even heard the word revision before.
Dr. Romond explained that my hip prosthesis had moved down into my femur, and it needed to be replaced. He told me he could not do the revision, because he had not done enough of them. “I want you to see Dr. John Heiner at the University of Wisconsin in Madison. He does revisions all the time.”
I reluctantly and fearfully agreed to go. When the day of surgery arrived, Dr. Romond cleared his patient schedule and was granted permission to observe my hip revision surgery at the University of
Wisconsin. What a comfort to know my local orthopedic surgeon was there in the operating room, too.
In 2007, when my left hip revision was done, Dr. Romond again traveled to UW-Madison and also observed that surgery.
John Heiner, MD, is a specialist in orthopedic oncology and adult reconstructive orthopedics at UW Health in Madison. Initially, I was afraid to see him, but my fears were totally unfounded. Dr. Heiner’s ability to relate as “just a regular guy” and intersperse wit and humor in his interaction with patients is a true gift.
After my second hip revision in 2007, I asked Dr. Heiner if my new revisions would last until I died.
With a gleam in his eye, he quickly replied, “If you tell me when you’re going to die, I’ll tell you if they will last!”

Jorge Casas-Ganem, MD, Sarah Troxell and Jennifer Reed, PA.

Sarah Troxell and her granddaughter, Kate Laster.

Sarah Troxell, her son, John, and husband, Gary.
My left hip revision lasted eight years, but then developed an infection, which had to be dealt with. For almost two years, from 2015–17, I had a draining wound in my left upper thigh. It was biopsied, incised and drained, packed, and again incised and drained, with only brief periods of closure. I was also seen at a wound clinic, where treatment continued without success. Finally, a sinogram and computed tomography scan revealed two abscess cavities, connected by a sinus tract, inferior and medial to the inside angle of my left hip prosthesis. A second cavity was located above and lateral to the acetabular component of my prosthesis.
I was now living in Texas, so I could not return to Wisconsin to have Dr. Heiner treat this infection. Instead, I was referred to Jorge Casas-Ganem, MD, of Dallas, an orthopedic surgeon who treats joint infections and performs revision surgery. When local doctors are uncomfortable treating a complicated patient, Dr. Casas is their choice. Certainly, I am known as a complicated patient.
On Oct. 10, 2017, Dr. Casas performed surgery on my left hip prosthesis and replaced the titanium cup, the polyethylene liner and the titanium femoral head. The femoral rod remained. Coagulase negative Staphylococcus epidermidis was identified in the cultures taken from the prosthetic components, and I was given appropriate intravenous antibiotic treatment as an inpatient, which continued as an outpatient.
At the present time, I continue on oral doxycycline hyclate 100 mg b.i.d. I remain under the care of Dr. Casas, who is one of the most meticulous physicians I have ever met. On my surgery date, he refused to proceed with my surgery until he had every type of prosthetic part available to choose from. I am certain this contributed to my successful surgery.
Eyes: For the past year, I have experienced yet another effect of my RA. In November 2016, the sclera of my left eye became very reddened, and I had extreme photophobia. Shortly after this, my right eye also developed redness. I was seen by ophthalmologist Richard Moore, MD, who diagnosed me with episcleritis. I am using prednisolone acetate 1% ophthalmic suspension, and this has successfully brought the inflammation under control. I continue under his care.

Sarah Troxell and her daughter, Laura Laster.

Sarah Troxell and John Heiner, MD.

Sarah Troxell and Jennifer Billodeaux, MPT.
Dr. Moore has included my rheumatologist, Dr. Heidi Schneider, in his treatment plan; he knows my history and understands the link between RA and eye inflammation. This is an example of two specialists working together to benefit the patient.
Rehab: Rehabilitation has also played an integral part in my life for the past 40 years. Both physical and occupational therapists have helped me regain strength and mobility, as well as improve daily function. Most recently, Jennifer Billodeaux, MPT, has been a great help to me by encouraging me to work hard to increase my walking ability. She carefully considered all of my diagnoses and then designed an exercise program to allow for my limitations. Jennifer has been able to instill an attitude of “Yes, I can do this” when I thought I could not.
An exemplary physical or occupational therapist knows when to encourage the patient while at the same time being realistic. Once I commented, “Look at how effortlessly those women walk on the track. I’ll never be able walk like they do.”
Jennifer was quick to reply, “But remember, Sarah, they have not had all the hip replacements or lived with all the chronic illnesses that you have.” She was absolutely right! I am glad that I can still walk at all.
Family Support Remains Key
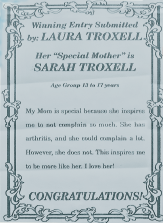
Mother’s Day article about Sarah Troxell, written by her daughter, Laura.
In addition to all of the healthcare professionals who have affected my life, my family members have cared for me, loved me and accepted me despite all of my limitations. My daughter, Laura, was born four years after my RA diagnosis. She grew up with a mother who had pain, numerous surgeries and needed help doing many daily tasks. Laura entered and won first place in a Mother’s Day contest when she described me as inspirational in my approach to living with RA. Even as a young adult, she offers to help me and teaches her children to look for ways to meet the needs of others.
My granddaughter, Kate, once told me, “You have a lot of things wrong with you, but you’re still a good grandma!”
My husband, Gary, has helped care for me for the past 40 years, performing everything from packing my thigh wound nightly for almost two years to cooking meals, house cleaning and emptying commodes. He is known as the “caregiver extraordinaire” to our friends, who marvel at his attitude and willingness to serve. As all of my doctors and therapists know, Gary can be found always at my side in the hospital or at any appointment.
I am truly blessed to have been assigned a life of living with RA. Without this difficult life, I would never have met so many amazing people, nor would I have been able to touch the lives of others for the past 40 years.
Sarah Troxell, RN, BSN, was the nurse coordinator and patient educator for the Coordinated Rheumatology and Pain Management Programs at Mercy Medical Center in Oshkosh, Wis., until her retirement. She is an emeritus member of the ARHP. She now resides in Longview, Texas.
Don’t miss these other articles by Sarah Troxell, in which she shares advice for rheumatologists and patients alike..
- Lessons Learned from a Patient with Rheumatoid Arthritis
- Advice Rheumatologists Can Share with Patients Planning to Relocate, a Patient Perspective
- Rheumatoid Arthritis Patient Shares Lessons Learned from Breaking Leg in a Fall

