
SAN FRANCISCO—At the May 17 California Rheumatology Alliance 10th Annual Medical and Scientific Meeting, Bevra H. Hahn, MD, professor emeritus of medicine, David Geffen School of Medicine, University of California Los Angeles (UCLA), gave a comprehensive talk titled, 2014: An Update on Pathogenesis, Diagnosis and Treatment of SLE.
She discussed two important new clinical concepts in systemic lupus erythematosus (SLE). First was the 2012 publication of the Systemic Lupus International Collaborating Clinics (SLICC) criteria,1 which have “definite advantages,” said Dr. Hahn, due to expansion of dermatologic, neurologic and immunologic disease classification indicators. The SLICC criteria, she said, have been validated in a cohort of more than 1,700 patients with lupus and shown to have 93% specificity and 92% sensitivity. Dr. Hahn has been encouraging pharmaceutical companies to incorporate these criteria along with the older ACR SLE criteria in clinical studies going forward.
The second clinical concept is the current international movement to incorporate treat-to-target (T2T) principles into management of people with lupus. “In my opinion,” she stated, “we need to do a better job [of treating patients]. That’s why we’re trying to introduce ‘treat to target.’ We should first treat to low level disease activity [LL-DAS, a concept introduced by the Asia Pacific League of Associations for Rheumatology and a EULAR committee] and then treat to prevent flares.” The goals of therapy should be to induce and maintain improvement, prevent damage and address pain, fatigue and depression, “which are major drivers of quality of life.” In conversation following the meeting, Dr. Hahn said she currently incorporates discussion of T2T in all her lupus talks and hopes that the U.S. rheumatology community will soon embrace the principles, which have been used successfully in rheumatoid arthritis.
Disease Pathways
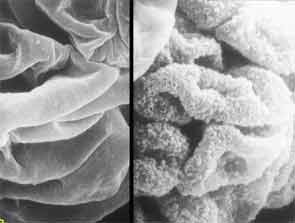
Dr. Hahn described the SLE disease process, which begins with autoantibodies and immune complexes fixing to tissue and causing damage by activating the complement system (a component of the innate immune system). The resultant inflammatory response takes on “a domino effect.” Recent research has revealed that neutrophils in the process of netosis cast out nets of protein studded with DNA, which present to the immune system, activating additional inflammatory response. Dendritic cells also sense the neutrophil nets and react by releasing interferon alpha. “We never thought neutrophils were major players in SLE, but they are,” Dr. Hahn stated.
Researchers now know of 50–55 genes that predispose people to SLE; and environmental factors, such as Epstein-Barr virus and cigarette smoking, are now well validated as possible triggers for lupus. Female gender is also important. Dr. Hahn also noted, “If lupus begins when the patient is younger than 25, it’s far more severe.”
Treat Nephritis Early
A heterogeneous disease, lupus has many organ manifestations. The kidneys are susceptible to damage, and the extent of involvement determines treatment strategies. It’s critical to recognize and treat nephritis early, said Dr. Hahn. “Delay of treatment more than six months increases mortality fourfold; and data from Chan et al in Hong Kong suggest that a delay of three months before initiating treatment doubles mortality.”
The Hong Kong group’s immunosuppressant of choice is mycophenolate. After achieving response, they recommend continuing immunosuppressants for three years, as does EULAR, contending that there is a larger rate of flares if immunosuppression is discontinued after two years.2 In the U.S., ACR guidelines do not state how long immunosuppressives should be continued, because the evidence has not yet reached Level A or B, which both require more than one series.

As she reviewed a plethora of clinical studies, Dr. Hahn encouraged her colleagues to apply a judicious filter to their interpretation of current research. In general, mycophenolate mofetil is a good choice, in addition to glucocorticoids, for inducing and maintaining improvement in lupus nephritis (LN). More controversial is the selection of the “correct” dose of cyclophosphamide. For example, European studies have shown good results for low-dose cyclophosphamide in LN; and British nephrologist Liz Lightstone’s group has shown 80% partial remission at two years with a glucocorticoid-sparing regimen of mycophenolate and rituximab without daily glucocorticoid dosing.3 However, noted Dr. Hahn, approximately 90% of the patients in the latter series were older European Caucasians. Applicability of European and Asian studies to populations treated in the U.S., which include African Americans and Latinos, many of whom are younger and with more severe disease, does not necessarily follow. “We have to think of that when we wonder whether we can apply those data to our populations and abandon the older ways of treatments,” she said.
Kidney transplant is now a viable option for poor responders in LN, said Dr. Hahn, who recalled that when she first started practicing, LN patients were denied transplants on the grounds the “kidney would be wasted” due to the fear of recurrence. In fact, renal-transplant survival rates in patients with SLE are comparable to those in patients without SLE; rejection of graft is the same as in non-SLE patients; and recurrence of SLE is very low, at 3% (which must be confirmed with a renal biopsy).
Glucocorticoids & Cyclophosphamide
Dr. Hahn said that current wisdom dictates that daily prednisone should be kept at or under 6 mg/day to minimize side effects. Questions remaining about glucocorticoids in LN include whether initial IV pulses are necessary, whether long-term daily dose is necessary and what the best doses are for inducing improvement and tapering schedules.
Similarly, despite some short-term trials in African American and Latino patients showing response rates for low-dose cyclophosphamide combined with abatacept in LN, questions remain about the effectiveness of the biologics and combination therapies in all races. Dr. Hahn’s opinion is that abatacept can be a “viable option” for patients whose LN is severe. Other data on anti-CD22, ocrelizumab, suggest that background mycophenolate might be more effective but also more predisposing to infection than low-dose cyclophosphamide.
To a question about the cost of biologics from the audience after her talk, Dr. Hahn said that clinicians must look beyond the bottom line: “If in fact your intervention costs $30,000 a year, but people have a better quality of life for 20 or 30 years, that intervention might be cost effective.”
At the end of her talk, which preceded a luncheon held in her honor, session moderator Gary R. Feldman, MD, FACR, announced that the CRA would be funding a rheumatology fellowship in Dr. Hahn’s name.
Gretchen Henkel is a medical journalist based in California.
References
- Bruce IN, O’Keeffe AG, Farewell V, et al. Factors associated with damage accrual in patients with systemic lupus erythematosus: Results from the Systemic Lupus International Collaborating Clinics (SLICC) Inception Cohort. Ann Rheum Dis. 2014 May 16. pii: annrheumdis-2013-205171.
- Bertsias GK, Tektonidou M, Amoura Z, et al. Joint European League Against Rheumatism and European Renal Association–European Dialysis and Transplant Association (EULAR/ERA-EDTA) recommendations for the management of adult and paediatric lupus nephritis. Ann Rheum Dis. Nov 2012;71(11):1771–1782.
- Condon MB, Ashby D, Pepper RJ. Prospective observational single-centre cohort study to evaluate the effectiveness of treating lupus nephritis with rituximab and mycophenolate mofetil but no oral steroids. Ann Rheum Dis. 2013 Aug;72(8):1280–1286.
