It is becoming increasingly clear that the integrity of the blood–brain barrier is very important in SLE-related neuropathology, and the lack thereof may allow for pathogenic antibodies to attack the brain. Although antineuronal and antiribosomal P antibodies are rare in children, they may be directly pathogenic or an epiphenomenon of NPSLE. Anti-NR2 receptor antibodies recently have been implicated in apoptotic neuronal cell apoptotic death after binding to the N-methyl-D-aspartate receptor but, currently, the role of anti-NR2 antibodies in NPSLE development remains controversial.1 Antiphospholipid antibodies are also implicated in NPSLE. These antibodies likely produce disease through ischemia via thrombi and noninflammatory vasculopathy.
Diagnosis of Neurobehavioral Syndromes in Children
To date, there is no single reliable laboratory test for detecting a neurobehavioral syndrome associated with SLE. The diagnosis of an SLE neurobehavioral syndrome of an individual child is based on clinical, neurological, and rheumatological evaluation, serological testing, brain imaging, and formal neurocognitive testing; the latter is considered the criterion standard for diagnosing cognitive dysfunction in SLE. Often, there is more suspicion than true evidence that SLE might be the cause of a neurobehavioral syndrome in a child.
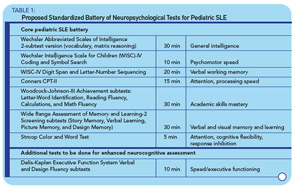
A recent survey among 128 pediatric rheumatologists indicates that 79% would consider performing formal neuropsychological testing for children with a history of overt CNS SLE (stroke, seizure, psychosis) and that 98% of providers would like to obtain formal testing for children with SLE who show academic decline or have cognitive complaints (patient or parent reports). However, besides widespread problems of access to formal neurocognitive testing, such testing is costly and may not be covered by insurance companies. Additionally, for children with SLE, there is no widely accepted standardized battery of neuropsychological tests that could be used as a gold standard for the diagnosis of cognitive dysfunction. This is because the ACR 1-hour Battery is not suitable for the testing of children. The Childhood Arthritis and Related Diseases Research Agenda (CARRA) Lupus Neuropsychiatric Working Group has developed a potential standardized battery, which is currently being tested for validity (see Table 1, below).
Computer-Based Neurocognitive Testing
Undoubtedly, the limited means of diagnosing cognitive dysfunction due to SLE leave many children at risk for remaining untreated for a disease manifestation that significantly decreases patient quality of life and worsens long-term prognosis. Current research is therefore exploring other testing modalities to facilitate recognition of this condition. For example, in adults with SLE, the Automated Neuropsychological Assessment Metrics (ANAM) has been successfully used to test the cognitive functioning of adults with SLE and children as young as 13 years of age (see Figure 1, left).
