A precipitous fall in erythrocyte sedimentation rate (ESR) despite persistently high C-reactive protein is another characteristic laboratory feature, which probably reflects the degree of hypofibrinogenemia secondary to fibrinogen consumption and liver dysfunction. In fact, liver involvement is common in MAS. Significant hepatomegaly is frequently present. Some patients develop mild jaundice. Liver function tests often reveal high serum transaminases activity and mildly elevated levels of serum bilirubin. Moderate hypoalbuminemia has been reported as well. Serum ammonia levels are typically normal or only mildly elevated.
Encephalopathy is another frequently reported clinical feature of MAS. Mental status changes, seizures, and coma are the most common manifestations of central nervous system disease. Cerebrospinal fluid pleiocytosis with mildly elevated protein has been noted in some studies. Significant deterioration in renal function has been noted in several series and was associated with particularly high mortality in one report.3 Pulmonary infiltrates have been mentioned in several reports, and hemophagocytic macrophages can be found in bronchoalveolar lavage.
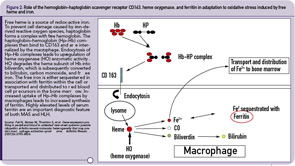
Additional laboratory findings in MAS include highly elevated serum levels of triglycerides and ferritin. The elevation of ferritin is particularly marked (above 10,000 ng/mL) in most patients and appears to parallel the degree of macrophages activation.
Diagnosis
There are no validated diagnostic criteria for MAS, and early diagnosis is often difficult. Thus, in patients with persistently active underlying rheumatologic disease, a fall in the ESR and platelet count, particularly in a combination with increase in serum D-dimer and ferritin levels, should raise a suspicion of impending MAS. The diagnosis of MAS is usually confirmed by the demonstration of hemophagocytosis in the bone marrow. However, the demonstration of hemophagocytosis in the bone marrow may be difficult due to sampling errors, particularly at the early stages of the syndrome. In addition, it is now increasingly recognized that hemophagocytic macrophages may infiltrate tissues other than bone marrow (e.g., liver, lymph nodes, skin, and lungs). In contrast to MAS, the diagnosis of HLH is usually established based on the validated diagnostic criteria developed by the International Histiocyte Society.9 The criteria include either:
- A molecular diagnosis based on specific mutations found in either PRF1 or MUNC13-4 genes; or
- A clinical diagnosis based on the following clinical criteria:
- Persistent fever;
- Splenomegaly;
- Cytopenias involving at least two cell lines;
- Hypertrigliceremia and/or hypofibrinogenemia;
- Hyperferritinemia; and
- Hemophagocytosis in the bone marrow.
More recently, two additional laboratory criteria have been added:
- Low/absent NK cell cytolytic activity; and
- High sIL2Rα levels.
The definite clinical diagnosis of HLH requires the presence of at least five of the eight criteria.