In December 2009, we encountered a 17-year-old male who was dying from a recently diagnosed catastrophic disease. He was previously healthy and athletic. He was a patient in the intensive care unit (ICU) with decompensated vital signs, following an exploratory laparotomy for polybacterial peritonitis and sepsis from gastrointestinal (GI) microperforations. He was deteriorating despite treatment with immune intravenous globulin (IVIG) and broad-spectrum antibiotics.
Prior to his presentation in the ICU, the patient had a two-year history of developing innumerable, multiplying avascular slightly depressed porcelain-like skin lesions surrounded by an erythematous rim. These were present primarily on his chest and abdomen. He was diagnosed with malignant atrophic papulosis (MAP), based on the skin biopsy findings and clinical history, in August 2009 (see Figure 1). Abdominal pain and other nonspecific GI symptoms had started six months earlier. Endoscopy was performed, which showed gastritis and an erythematous mucosa of the sigmoid colon, rectosigmoid junction and splenic flexure. Because of the severity of his pain, an exploratory laparotomy was performed, which showed multiple small 5–8 mm ulcerated lesions throughout the small bowel (see Figure 2). Further evaluation for an underlying rheumatologic disease was negative.

With the patient’s health steadily deteriorating, we desperately reached out to the medical community. We heard of a similar patient who had responded to treatment with eculizumab. We were able to obtain eculizumab on a compassionate-use basis, and he had an almost immediate response. Soon after, his abdomen was closed; it had been left partially opened due to abdominal compartment syndrome. Repeat echocardiogram showed resolution of the pericardial effusion, and the chest X-ray also showed improvement.
He continued to receive eculizumab infusions every other week and self-administered subcutaneous enoxaparin daily. He improved to the point that he gained back all the weight he had lost and was exercising again. Eventually, he returned to school, work and enjoying his life with family and friends.
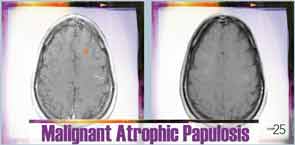
Six months after discharge, he developed gross hematuria and severe flank pain (enoxaparin was stopped). Cystoscopy demonstrated multiple lesions suggestive of MAP (see Figure 3). The dose of eculizumab was increased due to the concern that the dose reaching his bladder was subtherapeutic. The patient developed neurological symptoms, including perioral numbness and tingling sensation around his distal fingers. A magnetic resonance imaging (MRI) study of the brain was concerning for left frontal lobe vasculitis, as well as the presence of a 1 mm thick subdural hematoma. The dose of eculizumab was increased to weekly injections, and he was started on levetiracetam and aspirin.