The increased utilization of infusible biologics for the treatment of rheumatic diseases has opened the door for you to provide more integrated care for your patients. Having an in-office infusion center gives you the ability to deliver this service to your patients in a familiar and supportive setting, allowing you to direct the administration of the treatment rather than referring patients to the hospital. Another benefit of an onsite infusion center is increased patient adherence with medications and therapy. In addition, there is greater opportunity for patient interaction and education, which can strengthen the doctor–patient relationship.
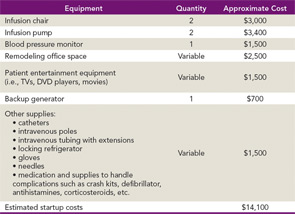
The process of operating an efficient infusion center involves creating an overall management strategy to evaluate areas such as staffing, general coding and billing, reimbursement methodologies, and financial obligations. The approximate start-up cost for an infusion center can range from $10,000–$15,000. Table 1 demonstrates an abridged list of necessary equipment and supplies you will need for your infusion center, along with approximate costs.
There are fixed costs, such as space rental, staff salaries, and healthcare benefits, which you will have to include with your start-up costs because these tend to make up a large part of practice management expenses. The cost of equipment can vary depending on vendors, so starting off on a smaller scale can usually keep costs in line with your budget.
Staff Requirements
Establishing an onsite infusion center may require hiring additional staff or training current staff members because you will need staff such as nurse practitioners, registered nurses, and physician assistants qualified to administer infusible drugs. Verify state licensure requirements for your health professional staff to work in the infusion center as state requirements vary. Additionally, staffing requirements can differ depending on how many patients your practice will infuse at the same time.
Billing for Infusion Drugs
There are two methods for obtaining medication for your infusion clinic. First, infusion medication can be acquired through the “buy and bill” plan under a patient’s healthcare plan. To use this method, you will have to establish an account with a wholesaler for specialty medication and purchase the drug from the vendor. Then you would bill the patient’s insurance plan. The second option, “assignment of benefits,” is typically covered under a patient’s prescription drug plan but requires preauthorization. This option necessitates using a specialty pharmacy to ship specific doses of medication for individual patients. Under this arrangement, the specialty pharmacy usually handles verifying patient insurance information and bills the patient for any copayment.
Carefully research how to acquire medications for your infusion center. Begin by examining your patients’ individual prescription drug policies and procedures, and then research various vendors to verify that you are getting the most competitive price on the drugs with guaranteed availability.
Coding for Infusions
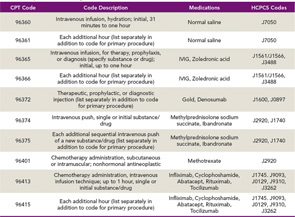
When coding for infusion services, there are specific coding and documentation guidelines to follow. Table 2 is a sample table for infusion code descriptors. Use the most recent CPT and HCPCS manuals to ensure you receive the correct reimbursement. Coding and billing staff must also be aware of code changes as well as any new categories for drug administration and infusions. Policy changes can be found on each carrier’s website under the medical policy section. Coding changes can be found in the newest CPT, ICD-9, or HCPCS books that come out each year.
There are specific coding rules for drug administration charges. For example, there can only be one initial code in the drug administration family, and all other codes must use a subsequent code. The supplies for local anesthesia, IV start, access to indwelling IV, subcutaneous catheter or port, the flush at conclusion of infusion, and standard tubing, syringes, and supplies are included in the relative value of the drug administration code and cannot be billed separately.
Infusion codes are based on time, so accurate documentation of the start time is strictly enforced. The documentation of time is essential for appropriate billing and reimbursement. See this month’s Coding Corner on page 18 for an example scenario. Also, download the ACR’s Rheumatology Coding Manual for more information on billing and coding specifically for rheumatology services at www.rheumatology.org/publications and click on Practice Management Publications.
Offering in-office infusion services for your patients has challenges, but it gives you the opportunity to provide the best standard of care at the point of service to your patients. It also opens the door for enhancing your practice through increased patient recruitment. For questions on coding and billing for infusion services, contact Melesia Tillman, CPC, CRHC, CHA, coding and reimbursement specialist, at [email protected]. For questions on the management of an infusion center, contact Cindy Gutierrez, insurance and practice management senior specialist, at [email protected].