ORLANDO, FLORIDA—Given the intersection between rheumatology and dermatology for many patients with autoimmune diseases, it’s helpful to hear from specialists in both fields regarding disease management strategies. With this in mind, the ACR Education Exchange 2023 session, Biologics Management of Psoriasis, provided a comprehensive and extremely helpful discussion of psoriasis treatment as seen through the eyes of an expert dermatologist.
ORLANDO, FLORIDA—Given the intersection between rheumatology and dermatology for many patients with autoimmune diseases, it’s helpful to hear from specialists in both fields regarding disease management strategies. With this in mind, the ACR Education Exchange 2023 session, Biologics Management of Psoriasis, provided a comprehensive and extremely helpful discussion of psoriasis treatment as seen through the eyes of an expert dermatologist.
Disease Severity
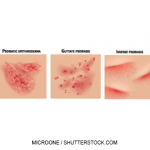
To begin his talk, Anthony Fernandez, MD, PhD, W.D. Steck Chair of Clinical Dermatology, Departments of Dermatology and Pathology, Cleveland Clinic, noted that psoriasis affects approximately 2–3% of the world’s population.1 Psoriasis represents a hallmark Th1/Th17 inflammatory disease, and the condition is related to an increased risk for a number of comorbidities. For example, severe psoriasis is an independent risk factor for myocardial infarction and stroke, and patients with severe psoriasis have a 57% increased risk of cardiovascular death, independent of traditional risk factors, over the general population.2 Evidence also suggests that patients with severe psoriasis may have a reduced life expectancy—five years shorter than age and sex-matched controls.3
Dr. Fernandez pointed out that various ways exist to grade disease severity in psoriasis, and many dermatologists begin by estimating the body surface area (BSA) involved. Using the palm of the hand (including the thumb) as a benchmark to represent about 1% BSA, clinicians can quickly determine approximate BSA involvement on the physical exam.
The National Psoriasis Foundation (NPF) grades BSA of <3% as mild, 3–10% as moderate and >10% as severe psoriasis. Although these measures are important, Dr. Fernandez noted that BSA may tell only part of the tale for patients. The specific anatomic areas involved and the physical symptoms associated with skin and nail findings make a big difference in quality of life for patients. For example, a patient with involvement of sensitive areas, such as the genitals, or very visible areas, such as the face, may believe their disease is severe even if the BSA involved is low. The psychological effects of psoriasis on patients are being recognized more and more, and this is an important part of the clinical evaluation and discussions with providers.
Dr. Fernandez reported that recent work from the International Psoriasis Council (IPC) has been helpful in creating a binary classification system that seeks to streamline access to systemic therapy for patients who previously may have been undertreated. Under the IPC schema, patients can qualify for systemic therapy if they fit into any of the following categories:
- They have tried and failed topical therapy;
- They have psoriasis involving the scalp, face, palms, soles, nails or genitals; or
- They have >10% BSA involvement.
The IPC hopes these criteria can be used to effectively identify patients who are suffering a reduced quality of life due to their disease and provide them with appropriate systemic therapy.
Treatment
In terms of the current psoriasis treatment landscape, Dr. Fernandez pointed out that 11 new biologic agents have been approved since 2004, including tumor necrosis alpha (TNF-α) inhibitors, interleukin 12/23 (IL-12/23) inhibitors, IL-17 inhibitors and IL-23 inhibitors.
Dr. Fernandez stated that the IL-23 inhibitors, in particular, were heralded as potential game-changing medications when approved because IL-23 is viewed as the master cytokine in the pathogenesis of psoriasis. Indeed, the data so far do not dispute the idea that IL-23 inhibitors may qualify as immune disruptors that can have significant disease-modifying effects.
In one study by Reich et al., researchers evaluated the five-year maintenance of clinical response and health-related quality-of-life improvements in patients with moderate to severe psoriasis who were treated with guselkumab, an IL-23 inhibitor. The researchers found that, after five years of treatment, more than one in two patients treated with guselkumab achieved complete resolution of psoriasis.4 Very few patients dropped out over the course of the study.
After five years of treatment, more than one in two patients treated with guselkumab achieved complete resolution of psoriasis.
Efficacy, as measured by Psoriasis Area and Severity Index (PASI) 90 and 100 scores, is being seen with risankizumab and bimekizumab as well.
For a systematic review of pharmacologic treatments of chronic plaque psoriasis, Dr. Fernandez described a Cochrane Review article on this subject published in 2022. This review indicated that IL-17 and IL-23 inhibitors may give patients the best chance of achieving PASI90. Overall, the most effective biologics for achieving PASI90 were infliximab, risankizumab, ixekizumab and bimekizumab, and the efficacy of each was similar when compared with each other. The authors of this review noted that, when taking into account the balance of efficacy and safety profile, risankizumab and bimekizumab appeared to perform the best.5
With all this in mind, Dr. Fernandez provided his personal opinion in terms of the treatment algorithm for managing patients with moderate to severe psoriasis who have no comorbid conditions, including no psoriatic arthritis. For these patients, he would typically use IL-23 inhibitors as first-line agents, followed by IL-17 inhibitors, IL-12/23 inhibitors and TNF-α inhibitors. He noted that, with IL-17 inhibitors, clinicians must be cautious of the increased risk for new-onset or flare of inflammatory bowel disease.
He went on to explain that the NPF recommends a treat-to-target approach in the management of patients with skin psoriasis, with the preferred target response being <1% BSA at three months and during the maintenance phase thereafter. An acceptable response is defined as <3% BSA or >75% BSA improvement with treatment.
Concluding Thoughts
To conclude his talk, Dr. Fernandez indicated two main questions still loom large in the field of psoriasis research:
- Does biologic therapy decrease the incidence of major adverse cardiovascular events (MACE)?
- Can biologic therapy prevent the future onset of psoriatic arthritis?
Both questions remain under active investigation, and for the latter question, a paper from Singla et al. provided interesting insights. The authors of this article found that in a large cohort study of patients with psoriasis, treatment with IL-12/23 inhibitors or IL-23 inhibitors was associated with a reduced risk of progression to inflammatory arthritis, compared with TNF-α inhibitors. This finding, if borne out by prospective observational cohorts and pooled analyses of previous randomized trials, may indicate the mechanism of action of treatment matters in potentially altering the future risk of psoriatic arthritis.6
Although this presentation did not delve deeply into the treatment of psoriatic arthritis, it was helpful to hear discussion of a dermatologist’s approach to the treatment of skin psoriasis.
Jason Liebowitz, MD, completed his fellowship in rheumatology at Johns Hopkins University, Baltimore, where he also earned his medical degree. He is currently in practice with Skylands Medical Group, N.J.
References
- Damiani G, Bragazzi NL, Karimkhani Aksut C, et al. The global, regional, and national burden of psoriasis: Results and insights from the Global Burden of Disease 2019 Study. Front Med (Lausanne). 2021 Dec 16;8:743180. eCollection 2021.
- Mehta NN, Azfar RS, Shin DB, et al. Patients with severe psoriasis are at increased risk of cardiovascular mortality: Cohort study using the General Practice Research Database. Eur Heart J. 2010 Apr;31(8):1000–1006.
- Abuabara K, Azfar RS, Shin DB, et al. Cause-specific mortality in patients with severe psoriasis: A population-based cohort study in the UK. Br J Dermatol. 2010 Sep;163(3):586–592.
- Reich K, Gordon KB, Strober BE, et al. Five-year maintenance of clinical response and health-related quality of life improvements in patients with moderate-to-severe psoriasis treated with guselkumab: Results from VOYAGE 1 and VOYAGE 2. Br J Dermatol. 2021 Dec;185(6):1146–1159.
- Sbidian E, Chaimani A, Garcia-Doval I, et al. Systemic pharmacological treatments for chronic plaque psoriasis: A network meta-analysis. Cochrane Database Syst Rev. 2022 May 23;5(5):CD011535.
- Schultheiss JPD, Brand EC, Lamers E, et al. Earlier discontinuation of TNF-α inhibitor therapy in female patients with inflammatory bowel disease is related to a greater risk of side effects. Aliment Pharmacol Ther. 2019 Aug;50(4):386–396.
Related Article
“Rheumatology Drugs at a Glance, Part 2: Psoriasis” May 17, 2019