For Daniel Albert, MD, a rheumatologist with the Dartmouth-Hitchcock Medical Center in Lebanon, N.H., some of his most defining medical experiences haven’t taken place within his practice, but in exotic locales such as a rainforest on the island of Borneo.
One of many physicians across the world who volunteer their time and expertise on medical missions, Dr. Albert recently wrote a book about his experiences, titled Volunteer, and he says the broad training rheumatologists receive in internal medicine and their ability to look at patient problems in an analytic manner make them great candidates to serve on medical missions.
“My first medical mission was in 1978, and since then I’ve participated in a dozen missions all over the world,” Dr. Albert says. “Each one is unique, and the work varies based on the country and the organization hosting the mission.”
Medical missions are typically offered in developing countries that have a shortage of physicians, and in areas that offer little access to healthcare. Dr. Albert says in some countries, rheumatologists may work in more of a primary care capacity, and in others, doctors specifically treat patients with rheumatic diseases. Many missions also use physicians as teachers and mentors, relying on them to share their expertise with doctors and medical students in the country they visit.
According to Dr. Albert, medical missions offer rheumatologists a different perspective on patient care, and allow them the opportunity to explore different cultures, gain a renewed energy for their profession and meet medical colleagues from all over the world. “You get to work with people you might never otherwise meet,” Dr. Albert says. “Serving on a medical mission is a valuable experience, and I think it makes you both a better person and doctor.”

Dr. Mallay has worked numerous missions in Central America.

During a volunteer mission in Guatemala, people lined up for hours to see a doctor.
The most common medical conditions seen on missions include hypertension, arthritis, asthma, migraines and diabetes, but Dr. Albert says doctors also treat medical conditions not typically seen in the U.S. “In Africa, for example, we saw patients with malaria, meningitis, pneumonia and infectious diseases, such as yellow fever,” he says.
Rheumatic diseases, such as rheumatoid arthritis (RA), also commonly occur in developing countries. A study published in the South Sudan Medical Journal found that “in countries where medical resources are limited, recognition and aggressive management of patients with RA may lag behind the treatment of infectious diseases associated with high mortality, such as malaria, tuberculosis, HIV and cholera.”1
In Borneo, Dr. Albert and his colleagues treated patients who had sustained injuries in car accidents, and in Uganda, he worked with a referral hospital to help start a rheumatology clinic and teach local medical residents about rheumatic diseases in a didactic forum. In Rwanda, Dr. Albert served on a medical mission in which he and his colleagues saw many patients with swollen and painful joints.

Volunteer doctors busy at work in the mountains of El Salvador, performing everything from blood pressure checks to minor surgeries.

In El Salvador, Dr. Mallay’s volunteer group set up its own makeshift clinics.
“We set up a field hospital [a small medical facility that takes care of patients on site],” Dr. Albert says. “It was during the civil war in Rwanda, which was rough. In situations like that, you learn a lot about yourself and how to do the best you can and improvise with the supplies you have.”
With technology lacking in some developing countries, Dr. Albert says routine diagnostic tests, such as a complete blood count (CBC), are often performed manually using a light microscope and a specialized microscope slide. In many countries, the working conditions can be less than ideal. Monitoring equipment, if available, may be outdated or only partially functional.
“You learn to work with the tools you have and to tolerate the limitations imposed on you,” Dr. Albert says. “Most of the doctors we work with in developing countries are very smart doctors who have learned to treat a vast array of medical conditions.”
A Once-in-a-Lifetime Experience
Rubaiya Mallay, MD, a rheumatologist at Suncoast Internal Medical Consultants in Largo, Fla., began serving on medical missions while attending medical school at the Edward Via Virginia College of Osteopathic Medicine in Blacksburg, Va. Traveling on medical missions to El Salvador, the Dominican Republic, India and Guatemala, Dr. Mallay says she and her colleagues not only diagnosed arthritis in many patients, but also worked to educate them on how to manage their condition.
“We saw a lot of patients who had arthritis due to years of working at jobs that required them to lift and carry heavy objects,” Dr. Mallay says.
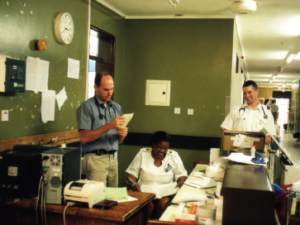
Dr. Albert worked with a volunteer team in Princess Marina Hospital in Gaborone, Botswana.

Following the 2004 tsunami disaster in India, Dr. Mallay joined a relief team that was one of the first groups to help the victims in Chennai, India.
In addition to diagnosing their condition and offering them steroid injections and anti-inflammatories, Dr. Mallay and her colleagues worked to educate patients on how to lift correctly and not exacerbate disease activity. They also gave out information on stretching exercises that could improve stiffness and range of motion.
“People would bring us food to show their gratitude and walk for miles to come to the mission clinics,” Dr. Mallay says. “Practicing medicine on a mission makes you more empathetic and very appreciative of everything we have in the United States.”
Each medical mission is unique, Dr. Mallay says. She’s treated children suffering from malnutrition and adults with undiagnosed diseases such as Parkinson’s, and worked to provide vaccinations to children and prenatal care to expectant mothers.
Dr. Mallay says the medical missions she’s embarked on have all partnered with local health professionals in developing countries to stress continuity of care.
“I think the most successful medical missions are those that are sustainable and continue to provide patient care long after the mission has ended and the medical volunteers have returned home,” she says. “Treating chronic conditions requires continuity of care, so it’s important for medical missions to partner with health professionals based in the [mission’s] country.”
Linda Childers is a health writer located in the San Francisco Bay area.
Finding Your Medical Mission
Dr. Albert says some of the best places to locate high-quality, affordable medical missions are through local universities or big nonprofit organizations. Doctors with a religious affiliation can typically locate medical trips through their church.
He says rheumatologists should consider the following questions before embarking on a medical mission:
What Kind of Care Will You Provide?
Rather than looking at medical missions that offer only a brief point of contact for patients, seek out missions that offer continuity of care and work to empower and educate patients, Dr. Mallay recommends. “Look for organizations that coordinate with local service agencies to best serve the medical needs of people in remote and very poor urban and rural areas,” she says.
What Types of Conditions Will You Primarily Treat?
If you want to work strictly on rheumatology cases, consider medical missions that specifically provide this care. For example, La-Merced.org (la-merced.org) focuses on medical missions to Nicaragua, and at the Roberto Clemente Clinic, its teams treat arthritic shoulders and knees with steroid injections and educate patients on how to better manage their arthritis.
What Are the Working Conditions Like?
Some medical missions believe in taking medicine to the people and providing care where there is none, because easy access to health clinics can often prove difficult for patients in developing countries. On these missions, volunteers set up makeshift clinics in remote villages, often in rugged conditions. If not having access to certain medical equipment or working in primitive facilities sounds problematic to you, Dr. Albert recommends finding a trip that operates in a more urban setting.
Does the Mission’s Country Present Unique Challenges?
Before embarking on a medical mission, Dr. Albert conducts due diligence on the country he plans to visit, and he makes sure he’s up to date on vaccinations. “In addition to helping others, you need to be cognizant of your own health,” he says. “In tropical areas, you can see cases of malaria and dengue fever. Tuberculosis is also common in many countries.”
For example, the Centers for Disease Control and Prevention (CDC) recommend (wwwnc.cdc.gov/travel) getting vaccinated for hepatitis A and typhoid if you travel to Haiti because travelers there can acquire both diseases through contaminated food or water.
How Long Is the Mission?
Some organizations, such as International Medical Relief, offer three-day mini missions for those who don’t have the time or financial resources to commit to a 10-day trip (internationalmedicalrelief.org).
Are There Non-Medical Opportunities for Your Family?
If you want your partner or family member(s) to travel with you, IMR offers opportunities for non-medical volunteers. These positions include trip historian, interpreter and community education class trainer/director.
What About Here at Home?
Volunteer doctors are often needed on domestic medical missions within the United States after natural disasters, such as the recent hurricanes in Florida, Texas and Puerto Rico. To learn more, visit the American Red Cross or the Medical Reserve websites.
Reference
- Radis C. Rheumatoid arthritis: Diagnosis and treatment with a particular emphasis on South Sudan. South Sudan Medical Journal. 2012 Nov;5(4).85–88.



