Image Credit: POPTIKAR/SHUTTERSTOCK.COM
Physician burnout is high and climbing. A 2015 report published by Medscape showed that nearly half (46%) of physicians surveyed responded that they were experiencing burnout; that number is up from 39.8% reported in a similar survey in 2013.1
These physicians experience the tell-tale signs of burnout: loss of enthusiasm for work (or emotional exhaustion), feelings of cynicism (or depersonalization) and low sense of personal accomplishment.2 The toll burnout takes on physicians goes well beyond ill effects on professional and personal health, and may erode their ability to maintain allegiance to the Hippocratic Oath that anchors all physicians to place the needs of the patient first. With burnout comes the increased risk of medical error and a decrease in the quality of patient care.
Although frontline emergency room and primary care physicians have the highest rates of burnout, all physicians are at risk. It’s estimated that up to 60% of physicians will experience burnout during their careers.3
And it’s not just mid-career physicians who are burning out.
“Initially, it was thought that people begin to burn out in mid-career,” says Prashant Kaushik, MBBS, rheumatology lead physician/section chief, Stratton VAMC, and associate professor and program director for the Rheumatology Fellowship Department of Internal Medicine, Albany Medical College, Albany, N.Y. “That is a myth. Medical students, residents, fellows and, of course, practicing physicians in all levels of their career are burning out.”
Rheumatologists are no exception. The Medscape survey showed that 43% of rheumatologists reported burnout in 2015.1
What leads to burnout, and what is being done about it?
Causes
“The most important factor [leading to burnout] may be that we are addressing crisis after crisis after crisis day in and day out,” says Luke Fortney, MD, a family medicine doctor with Meriter Medical Group, Madison, Wis. “This alone can be fatiguing, and then add in a feeling of professional isolation, and burnout can exacerbate.”
Other common factors affecting burnout are increased bureaucratic tasks, long work hours, insufficient income, increasing computerization and documentation of clinical practice, and effects of the Affordable Care Act, which has provided needed insurance to many previously uninsured people while flooding an already overextended healthcare system with more patients.1
None of this may be new or news to the physician in the clinic. What may be new is what is being done to address this pervasive problem.
Time for the Mind
Just as the foundation of medicine is built on the work and thought of the ancient Greeks, a way to manage burnout is emerging that has an even older influence—the way of meditation, or in more contemporary parlance, mindfulness or mindfulness meditation.
Evidence is mounting on the effectiveness of meditation to reduce or counter the effects of burnout.3,4,5 Data from a 2009 study show that primary care physicians who participated in a continuing medical education (CME) course that included mindfulness meditation had both short- and long-term improvements in well-being and attitudes, such as empathy associated with patient-centered care.5 More recent data show that participation in an abbreviated training course on mindfulness intervention (eight weeks) for primary care physicians led to reductions in depression, anxiety, stress and indicators of job burnout.3 A follow-up study showed feasibility and success in cultivating mindful awareness training in the healthcare system.4
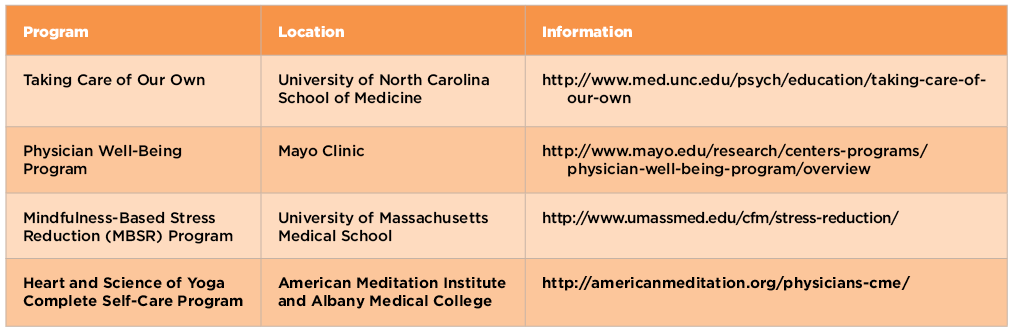
Currently, a number of CME programs that train physicians in meditation are now being offered around the U.S., as well as online (see Table 1).
Dr. Kaushik, who employs many yoga self-care practices at the Stratton VA Medical Center in Albany, says that meditation, gentle yoga and diaphragmatic breathing used to prevent and relieve burnout are available to meet the needs of physicians and, in particular, are available to work within the constraints on physicians’ time.
For six years, Albany Medical College, in joint providership with the American Meditation Institute (AMI), has presented comprehensive training in yoga science as holistic mind/body medicine to relieve physician burnout. Now in its seventh year, this year’s conference will be held Nov. 3–7, 2015, at the Cranwell Resort in Lenox, Mass.

Dr. Kaushik
Dr. Kaushik, who will be lecturing on the use of simple yogic techniques, such as mantra meditation and diaphragmatic breathing to relieve burnout, says the course will provide practical instruction for physicians and other healthcare professionals on meditation skills by providing them an entire toolbox of techniques they can use in their personal and professional lives.
Along with the annual November conference, the same curriculum is available throughout the year in different formats, including a six-week program at the AMI near Albany and a summer weekend retreat every July.
Joel Kremer, MD, Pfaff Family Professor of Medicine at Albany Medical College and director of research, The Center for Rheumatology, Albany, N.Y., who has attended the annual CME meeting at AMI, emphasized the importance for physicians to have an open mind to alternative methods to relieving stress while recognizing the challenge of finding time to do it. “There is a Catch-22,” he says. “We [physicians] are too busy to consider and be educated about alternative methods for relieving stress.”
Dr. Fortney agrees. “Challenges include adding yet another thing to a physician’s endless and growing list of things to do,” he says. Dr. Fortney also emphasizes that meditation may not be for everyone, but other ways may provide similar benefits.
“Whether a person meditates every day or goes for a walk through the woods would be an individual choice, but in general, time is a major factor,” he says.
Dr. Kaushik puts it differently. “Meditation is a dire necessity,” he says. “It is the only way to change the software of the mind so that we can absolutely alleviate physician burnout.”
Mary Beth Nierengarten is a freelance medical journalist based in St. Paul, Minn.
References
- Medscape Physician Lifestyle Report 2015. Medscape Multispecialty. 2015 Jan.
- Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012 Oct 8;172(18):1377–1385.
- Fortney L, Luchterhand C, Zakletskaia L, et al. Abbreviated mindfulness intervention for job satisfaction, quality of life, and compassion in primary care clinicians: A pilot study. Annals of Family Medicine. 2013;11(5):412–420.
- Luchterhand C, Rakel D, Haq C, et al. Creating a culture of mindfulness in medicine. WMJ. 2015;114(3):105–109. .
- Krasner MS, Epstein RM, Beckman H, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA. 2009 Sep 23;302(12):1284–1293.