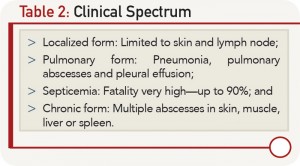
The disease spectrum is variable, and the infected individual can remain a carrier with totally asymptomatic infection or remain latent for years and manifest whenever cell-mediated immunity is suppressed. Melioidosis is known to present as a febrile illness, ranging from an acute fulminant septicemia to a chronic, debilitating localized infection and abscess formation (see Table 1, and Table 2).
The common portals of entry of B. pseudomallei are inoculation through minor skin abrasions, inhalation and ingestion. The normal incubation period in cases of melioidosis ranges from 1–21 days (mean nine days). The longest recorded apparent incubation period is 61 years.
Septic arthritis and osteomyelitis are rare, but well-recognized, forms of the disease.3,4 Generally, septic arthritis arises from the hematogenous dissemination of the organism, but it may follow direct spread from other organs or soft tissue infections over joints. Large joints, such as the knee, ankle, elbow or shoulder, are usually involved in this disease. The most commonly affected joints are the knee and shoulder.4 Melioidotic septic arthritis is often seen in patients with chronic diseases, including diabetes mellitus, chronic renal failure, cirrhosis, systemic lupus erythematosus and malignancies.3,4 Kosuwon et al found that diabetes mellitus was a predisposing factor in the majority of patients with septic arthritis.4
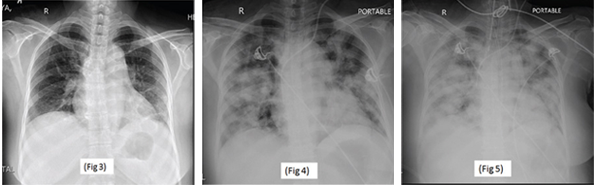
Serial chest X-rays: on the day of admission (Fig. 3), on the third postoperative day (Fig. 4) and on the fourth postoperative day (Fig. 5).
A delay in diagnosis can be fatal, because empirical antibiotic regimens used for suspected bacterial sepsis often do not provide coverage of B. pseudomallei. A culture of B. pseudomallei from any clinical sample is a sine qua non for diagnosis of melioidosis. Gram stain of synovial fluids is a quick approach, but the identification of gram-negative bacilli with bipolar staining is infrequent. Latex agglutination test based on polyclonal or specific monoclonal antibodies to lipopolysaccharide or exopolysaccharide can, therefore, be undertaken for definitive identification.2 Serological tests,
such as enzyme-linked immunosorbent assay, to detect immunoglobulin M and immunoglobulin G antibodies, and molecular methods (e.g., polymerase chain reaction) are also used for definitive diagnosis of disease.1,2
B. pseudomallei is inherently resistant to ampicillin, penicillin, first- and second-generation cephalosporins, gentamycin, tobramycin, streptomycin and polymyxin.1,2 Treatment consists of two phases:
- Intensive phase consisting of 10–14 days’ treatment with ceftazidime, imipenem or meropenem given parenterally.
- Oral eradication phase with three to six months of trimethoprim-sulfamethoxazole.1,2
Even with optimal treatment, the mortality from acute severe melioidosis is high (30–47%), as in our case.