SNOWMASS, CO—The go-to medication for treating rheumatoid arthritis (RA)—methotrexate—also has potential for mitigating inflammatory bone disease, according to Bruce Cronstein, MD, Paul R. Esserman professor of medicine, director of NYU-HHC Clinical and Translational Science Institute in New York City, who presented Taking a Bite Out of Inflammatory Bone Disease at the ACR’s Winter Rheumatology Symposium this January. During his presentation, Dr. Cronstein reviewed the biology of bone homeostasis and discussed how regulating certain molecules may reduce bone destruction in inflammatory arthritis, as well as in inflammatory osteolysis in prosthesis loosening.
Osteoneurology & Axonal Guidance Proteins
The foundation of osteoneurology is that neuronal mediators regulate bone homeostasis, Dr. Cronstein said. Adenosine receptors (A1, A2A, A2B and A3) play a key role in the central nervous system, where they were first described. Specifically, A1 receptors mediate sedation and sleep, and A2A receptors are involved in coordination. A2A receptors also inhibit osteoclast differentiation and stimulate osteoblast expression of axonal guidance proteins, which further regulate osteoclast differentiation.
Dr. Cronstein gave several examples of axonal guidance proteins that have roles in bone homeostasis, including netrin-1, semaphorin 4D (Sema4D) and semaphorin 3A (Sema3A). Axonal guidance proteins are also known to “mediate osteoclast–osteoblast interactions in inflammatory bone lesions,” Dr. Cronstein added.
Netrin-1 is a chemorepulsant that plays a role in immunity and inflammation and is required for osteoclast differentiation. Stimulation of adenosine A2A receptors inhibits expression of netrin-1 and its receptor Unc5b during osteoclastogenesis, and blocking netrin-1 or Unc5b diminishes inflammatory bone destruction.
Sema4D is secreted by osteoclasts and inhibits osteoblast bone formation, whereas Sema3A is secreted by sensory neurons and osteoblasts, and inhibits osteoclast differentiation. Like netrin-1, both are specifically affected by adenosine receptors. Laboratory studies show that adenosine receptors suppress Sema4D expression by osteoclasts, which potentially stymies bone loss, and stimulate Sema3A expression by osteoblasts, which potentially promotes bone growth. Because of this link, Dr. Cronstein said, axonal guidance proteins may be novel targets for the treatment of bone disease.
Further, Dr. Cronstein said, research has shown that Sema3A regulates bone mass accrual through sensory innervations.1 The researchers noted that in animal models, Sema3A is abundantly expressed in bone, and it affects osteoblast differentiation. They tested several cases in mice, including Sema3A knockout mice, osteoblast-specific Sema3A-deficient mice, and mice lacking Sema3A in neurons. Based on their results, the researchers concluded the Sema3A that regulates bone density is made by the peripheral nerves.
Biology of Inflammatory Bone Disease
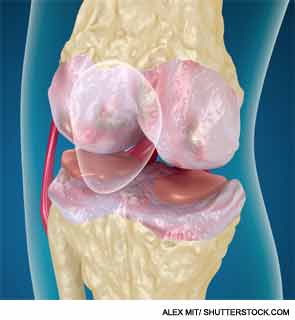
In patients with inflammatory processes, such as RA or osteoarthritis (OA), the balance between osteoblasts and osteoclasts tips, leading to increased bone loss. By regulating the molecules that promote or inhibit osteoclast/osteoblast processes (e.g., differentiation, communication), it’s possible to mediate bone loss, Dr. Cronstein said.
In established inflammatory bone disease, there is an increase in osteoclasts, B cells, T cells and TNF. These cytokines and other inflammatory cytokines have been shown to contribute to inflammation in RA and other inflammatory diseases, Dr. Cronstein said.
During osteoclast differentiation, one receptor that is particularly noteworthy is receptor activator of nuclear factor–κB (RANK) and RANK-ligand (RANKL).
“[Osteoclasts] express this receptor called RANK and [RANKL], which is a protein that’s expressed on the surface of osteoblasts, and there’s also a soluble form,” Dr. Cronstein said. “This is one very well worked out way that osteoblasts talk to osteoclasts. Either the RANKL on the surface of osteoblasts or the soluble form binds to the receptor on the osteoclast precursors, and that induces differentiation to form osteoclasts.”
Of note, RANKL antibodies can be used to inhibit bone turnover and treat very severe forms of OA, Dr. Cronstein said.
In addition to RANK and RANKL, the communication between osteoblasts and osteoclasts involves several other molecules, including Sema4D–plexin-B1 and TGF-β1. “Sema4D is a molecule made by osteoclasts that turns off osteoblasts, and there are many other molecules that have similar types of functions.” One such molecule, TGF-β1, is one of the basic growth factors that’s suppressed in the body and is required for growth of many different kinds of tissues.
By regulating the molecules that promote or inhibit osteoclast/osteoblast processes (e.g., differentiation, communication), it’s possible to mediate bone loss.
Adenosine & Methotrexate
Another key component of bone homeostasis is adenosine, which contributes to intercellular communication via its four receptors. Of note, “the antiinflammatory effects of methotrexate are largely mediated by adenosine,” Dr. Cronstein said. “Adenosine, acting at its receptors, inhibits bony destruction in inflammatory arthritis.”
Further, he said, stimulating adenosine A2A receptors is known to inhibit osteoclast differentiation, whereas deletion of A2A receptors leads to increased osteoclasts and diminished bone density. The antiinflammatory effects of methotrexate related to inflammatory bone disease are mediated by adenosine in the following ways:
- Antagonism of A1 prevents osteoclast formation and function.
- Stimulation of A2A prevents osteoclast formation and function.
- Stimulation of A2B is critical for osteoblast differentiation.
“Bone destruction is mediated by the same cells that are normally present, you just get an exaggeration of the turnover component during inflammatory disease such as RA,” Dr. Cronstein said. “With methotrexate, adenosine can inhibit inflammation and bone destruction, and we’ve shown in models of inflammatory arthritis that methotrexate, working through adenosine, can inhibit the bone destruction that occurs.”
These antiinflammatory effects can be stymied, however. Caffeine and theophylline are adenosine-receptor blocking agents, Dr. Cronstein cautioned. They can “completely reverse” the antiinflammatory effects of methotrexate.
Inflammatory Osteolysis in Prosthesis Loosening
Adenosine-related mechanisms and axonal guidance proteins (i.e., Sema4D, netrin-1) may also be important in treating osteolysis in prosthesis loosening. Approximately 800,000 prosthetic joints are implanted annually in the U.S., Dr. Cronstein said. Despite changes in prostheses and surgical techniques, there has been no reduction in the rates of surgical revision—as many as 25% of patients undergo removal and replacements of the prosthesis. Inflammation caused by wear particles and osteoclast-mediated bone erosion are major contributors to prosthesis failure.
Laboratory studies show that adenosine receptors suppress Sema4D expression by osteoclasts. This is important, Dr. Cronstein noted, because Sema4D is highly expressed in periprosthetic soft tissue in patients who require prosthesis revision. Netrin-1 is similarly overexpressed in this case.
Stimulation of adenosine A2A receptors diminishes netrin-1 expression during wear particle–induced bone resorption. Stimulation of A2A can also suppress inflammatory bone disease by inhibiting osteoclast formation and function, stimulating interleukin (IL) 10 and osteoprotegerin expression, diminishing RANKL expression and diminishing wear particle–induced osteolysis.
Methotrexate-induced adenosine specifically diminishes arthritis-associated bone disease, and because of this mechanism, it may also be a potential therapy for mediating the inflammatory osteolysis in prosthesis loosening. According to Dr. Cronstein, the positive effects of methotrexate due to its A2A receptor–mediated mechanism are that it diminishes wear particle–induced osteolysis and wear particle–induced suppression of bone formation.
Dr. Cronstein discussed recently published research that he and his colleagues conducted, showing additional potential for A2A in mitigating osteolysis.2 The researchers concluded, “These results in mice suggest that site-specific delivery of an adenosine [A2A receptor] agonist could enhance implant survival, delaying or eliminating the need for revision arthroplastic surgery.”
In their animal study, the researchers noted that applying an adenosine A2A agonist inhibits wear particle–induced bone loss, diminishes wear particle–induced inflammation, reduces the number of osteoclasts in treated bone and restores bone formation.
Kimberly J. Retzlaff is a medical journalist based in Denver.