Antibiotics: Another shotgun approach to altering the gut microbiota in rheumatic disease is the use of antibiotics. However, antibiotics may be a double-edged sword with respect to inflammatory arthritis. Several recent studies evaluating large European databases have shown that early use of antibiotics may be a risk factor for subsequent development of pediatric IBD and JIA.35-38 However, although antibiotics don’t appear to be effective in SpA, studies of their effect in adult RA patients have demonstrated success.39,40
The microbial counterpart to a deep bench is high alpha diversity, which is a measure of the richness, as well as the evenness, of the organisms present in a community. Specifically, richness speaks to the number of different organisms, while evenness speaks to their distribution. Thus, a balanced & diverse microbiota may be optimal for maintaining health.
It’s hard to imagine that a disease potentially caused by antibiotics (e.g., JIA) could then be treated by antibiotics. Moreover, the risks of long-term antibiotic use, such as infection with C. difficile, also discourage their use. Further, antibiotics are fairly indiscriminate in their effect on the microbiota, wiping out both beneficial and harmful organisms and undoubtedly adversely affecting diversity. There has been very little interest in their use in the biologic era, and at present, it is difficult to propose introducing them as part of the therapeutic armamentarium for children with JIA. However, the positive results of some of the studies in using antibiotics to treat rheumatic disorders speak to the potential of therapeutic alterations of the microbiome.
Diet: Perhaps, a safer approach to altering gut microbiota involves dietary changes. That dietary changes can rapidly effect alterations in the microbiome is well established. For example, the study by Wu and colleagues also involved an interventional arm, in which 10 subjects were randomized to either a low-fat or a high-fat diet for 10 days, with substantial changes seen in some subjects after just one day.10 In light of the typical American diet, the changes appeared to be more pronounced among those randomized to the low-fat diet compared with those randomized to the high-fat diet.
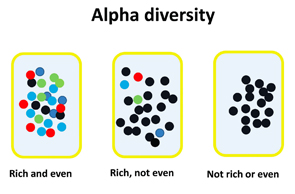
Figure 2: Illustration of the concepts of richness and evenness within alpha diversity. Richness refers to the variety of different organisms; evenness refers to the distribution of the organisms within the population.
An extreme form of dietary change consists of exclusive enteral nutrition (EEN), which appears to be comparable to corticosteroids as induction therapy in pediatric IBD.41 On the other hand, dietary interventions in RA have not been particularly effective.42 There are no data in children, aside from a case report of EEN benefit in a child with refractory polyarticular JIA.43 It must be emphasized that just because a particular diet may alter the microbiota, it does not follow that this alteration is beneficial with respect to any particular disease process. In addition, many diets may be very difficult to sustain. The challenge will be in identifying a diet that promotes beneficial changes in the microbiota, provides appropriate balanced nutrition and is acceptable to families for the long term.

