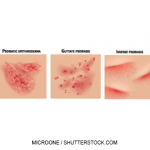
NEW YORK (Reuters Health)—The pathology of pediatric psoriasis differs from that of adult psoriasis, a finding that has implications for treatment, researchers suggest.
“Pediatric psoriasis often differs from adult psoriasis in presentation, triggers, natural history, and response to therapy, suggesting potential differences in the pathophysiology of the disease processes,” Dr. Kelly Cordoro of the University of California, San Francisco (UCSF) and colleagues observe in the Journal of the American Academy of Dermatology, online June 14.1
However, most studies examining the immunology of psoriasis have focused on adult patients. For the new research, the team used flow cytometry to characterize the inflammatory cell profiles of psoriatic plaques from pediatric patients and adult psoriasis skin obtained from the UCSF General Dermatology clinics. They also studied normal skin obtained from pediatric patients undergoing plastic surgical reconstructive or excisional procedures at from which benign normal tissue margins were available and would have otherwise been discarded, and normal, healthy adult skin obtained from patients undergoing elective surgery.
Ten pediatric psoriasis patients (eight boys, mean age 12) were included in the study. Most had mild psoriasis at the time of biopsy, but moderate to severe disease was reported by all but three patients at some point during the disease course. Two had ongoing moderate and one had very severe disease at the time of enrollment.
Lesional tissue from the pediatric patients had significantly increased IL-22 and significantly less elevation of IL-17 derived from CD41 and CD81 cells compared with tissues from adult psoriasis patients and pediatric controls.
Also in contrast to lesions from adults, lesional skin in pediatric patients did not have increases in regulatory T cells.
Dr. Cordoro tells Reuters Health, “This pilot study supports the notion that ‘kids are not just little adults’ when it comes to the immunopathology of psoriasis at the tissue level.”
“The results provide evidence that IL-22, in addition to and to a greater extent than IL-17, may be a major player in the pathologic mechanism of psoriasis in children,” she says by email.
“The overarching goal of research like this is to start a new era in which physicians are no longer forced to adapt knowledge gained from adult studies to the management of pediatric patients,” she stresses. “Our findings get us a step closer to unraveling the immunologic signature of pediatric psoriasis, which may reveal therapeutic targets unique to children.”
Dr. Adnan Mir, a pediatric dermatologist at Children’s Health in Dallas, tells Reuters Health by email, “Psoriasis often behaves differently in children and adults, and little is known about why that is the case. For example, psoriasis in children is often triggered by Streptococcal infections, such as Strep throat.”
“Despite the differences, we often treat adult and pediatric psoriasis using similar strategies,” he says.
“Over the past two to three decades, advances in the understanding of what causes psoriasis has led to the development of more sophisticated, targeted therapies—but these have, for the most part, been focused on adult disease,” he observes.
“This is an important study that addresses differences in adult and pediatric psoriasis at a molecular level,” he says. “This improved understanding of the cellular and molecular pathways that are active in pediatric psoriasis will help us to tailor our treatments specifically to this population, and lead to the development of newer, safer therapies.”
Reference
- Cordoro KM, Hitraya-Low M, Taravati K, et al. Skin-infiltrating, interleukin-22-producing T cells differentiate pediatric psoriasis from adult psoriasis. J Am Acad Dermatol. 2017 Jun 14. pii: S0190-9622(17)31735-8. doi: 10.1016/j.jaad.2017.05.017. [Epub ahead of print]