
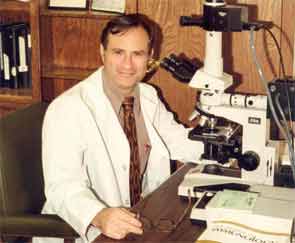


“Come to Oklahoma and have a good time!” Those were the words that persuaded John B. Harley, MD, PhD, to join Morris (“Moe”) Reichlin, MD, as a faculty member in Oklahoma City in the early 1980s, where Dr. Reichlin was busy establishing what would become a well-recognized rheumatology training program at the University of Oklahoma Health Sciences Center, as well as a world-class research program and clinical autoantibody testing facility at the Oklahoma Medical Research Foundation (OMRF). Dr. Harley, currently chief of pediatric rheumatology at the University of Cincinnati Children’s Hospital Medical Center, explains: “What Moe meant by ‘have a good time,’ of course, was to really enjoy the science.”
Dr. Reichlin’s infectious enthusiasm for conducting research has drawn countless pre- and postdoctoral fellows and colleagues to OMRF since 1981, when he and his wife Marianne and colleague Ira N. Targoff, MD, packed up their lab equipment and moved from Buffalo, N.Y., to Oklahoma City. Now a professor emeritus and affiliate of OMRF Arthritis and Clinical Immunology Research Program, Dr. Reichlin is known foremost in rheumatology and immunology circles as one of the discoverers of anti-Ro (SSA) antibodies—and as the man who put Oklahoma rheumatology research on the map.1 From its origins in 1981, the program has expanded from an initial 25 to 30, to a staff of nearly 200 individuals. “We had great success with our science, both nationally and internationally,” says Dr. Harley. “We worked really hard and, at the same time, we had a good time.”
Dr. Reichlin has been motivated during his more than five-decade-long, award-winning career by the quest to define the antigenic targets of autoimmunity in people with systemic lupus erythematosus (SLE), inflammatory myopathies, polymyositis, and dermatomyositis. Throughout that time, Dr. Reichlin also remained intimate with clinical work and teaching. “Patients were my guideline, in disease classification or characterization,” he says. “If it meant something to the patient, then it meant something to me, and I pursued it.”
A Path to Immunology
Dr. Reichlin says he always knew he would go into medicine. As an undergraduate, he majored in chemistry and believes it may have been his mother who had initially urged him to become a physician (“She was a very strong person,” he said). In the 1960s, he studied the immunochemical properties of hemoproteins, particularly hemoglobin and cytochrome c, honing his laboratory skills in the graduate department of biochemistry at Brandeis in Boston, and as a postdoctoral fellow of the National Institutes of Health (NIH) in biochemistry at the University of Rome.2-4 He developed reagents that could help distinguish a single amino acid difference in protein structure.5
His first mentor, Thomas B. Tomasi, MD, PhD, was a powerful influence during his years at the University of Vermont’s College of Medicine in Burlington: “I modeled myself after him,” says Dr. Reichlin; he followed Dr. Tomasi to the State University of New York at Buffalo in the mid-1960s. There he handled a demanding schedule, taking on dual appointments, moving from associate to assistant to full professorships of medicine and biochemistry. It was also in Buffalo that Dr. Reichlin began his studies to define antigenic targets reactive with antibodies in sera from patients with SLE.
Early on in his academic career, Dr. Reichlin’s research was intertwined with his clinical rheumatology work. “I was seeing patients with rheumatic diseases, and realized that there was a big gap in the knowledge of the chemistry associated with those syndromes,” he says. “It was an easy transition to do research on the chemistry of autoimmunity, which was obvious in all the connective tissue diseases, especially lupus, but also in inflammatory myopathy, scleroderma, and Sjögren’s syndrome.”
Patient-Oriented Science
Dr. Reichlin has mentored predoctoral and postdoctoral fellows who have established active research programs in the United States and around the world, imbuing in them the values of translational research. “He is the quintessential triple-threat rheumatologist,” says Judith A. James, MD, PhD, who came to OMRF as an undergraduate student in 1988, fully expecting to become a pediatric allergist and immunologist. She was so transfixed by the work she was doing in Dr. Reichlin’s and Dr. Harley’s laboratories that she changed the course of her own career, becoming a rheumatologist and following the academic American Board of Internal Medicine pathway. She was the first, with Dr. Reichlin’s encouragement and support, to come through the official MD/PhD program at the University of Oklahoma. In awe of Dr. Reichlin and his reputation when they first met, Dr. James notes that she has always appreciated his “interest in doing great science, and in understanding how this science would be directly relevant to patients.” Dr. Reichlin also emphasized “how important it was to have a broad exposure in science and clinical medicine,” she recalls. “You never knew where a lesson learned in another discipline might become directly relevant in rheumatology.” Dr. James is now program chair of the Arthritis and Clinical Immunology Program as well professor of medicine at the University of Oklahoma Health Sciences Center. When she became a faculty member, Dr. Reichlin transferred care of some of his patients to her, some of whom, after well over a decade, “still call themselves ‘Dr. Reichlin’s patients,’ ” she says wryly.
Setting the Tone
Dr. Harley was the first faculty member recruited to the OMRF arthritis program, an appointment made possible by an endowment to the foundation. As a leader, Dr. Reichlin “was supportive and didn’t interfere,” says Dr. Harley. “Presenting to him was always a great thing because he thought creatively, and was able to suggest the perfect experiment or interpretation of your data,” says Robert H. (“Hal”) Scofield, MD, who joined OMRF as a postdoc and then became a faculty member.
Dr. Scofield recalls many late afternoon sessions “planning and discussing our science. He set the tone that the program should be collegial and interactive.” Enjoyment of each other’s company was also part of the recipe. Dr. Harley recalls annual chili cook-offs every February in honor of Dr. Reichlin’s birthday, and during holiday gatherings at the Reichlin home, Drs. Scofield and Reichlin were known to perform on their trumpets (see photo at right). “I’m a social character,” says Dr. Reichlin. “I like to interact with people, and I feel that organizational skills are important in moving a field forward. So it came naturally and easily to me.”
Legacy of Generosity
“There wasn’t anyone who had more influence on my career than he did,” Dr. Targoff now says of his long-term association with Dr. Reichlin. After residency, he joined Dr. Reichlin’s research program in Buffalo. Then, when it was time to establish his own lab, Dr. Reichlin “made that transition very easy for me. He was also a good role model for academic medicine.” Currently, Dr. Targoff is an assistant member with the Arthritis and Clinical Immunology Research Program and professor of medicine at OHSC, and a staff physician with the Oklahoma City Veterans Affairs Medical Center.
Yasuhiko Itoh, MD, PhD, of the department of pediatrics at Nippon Medical School in Tokyo, did his postdoctoral work in rheumatology at OMRF from 1988 to 1991. “As a supervisor, Dr. Reichlin was incredibly patient and very good at praising young people. During my first month in the lab, I repeatedly failed Western blots. When I finally succeeded, he told me, ‘You are the King of Gel!’ ” Exposure to Dr. Reichlin’s autoantibody discoveries and research values have continued to influence Dr. Itoh’s own work, as he continues to try, he says, to “solve patients’ symptoms as scientifically as possible.”
Dr. Scofield notes, “Moe was always really generous with everybody, always wanting to collaborate and to nurture the next generation.” That trend has continued. In 2007, Yehuda Shoenfeld, MD, head of the Zabludowicz Center for Autoimmune Diseases in the Sheba Medical Center and Tel-Aviv University, Israel, whose laboratory is well known for experimental models of induced autoimmune disease, was interested in investigating the psychiatric manifestations of lupus. He contacted Dr. Reichlin, who immediately agreed to send purified anti-P ribosomal antibodies for the experiments, which involved injection of the autoantibodies directly to the brain to bypass the blood–brain barrier. The mice developed depression. In follow-up investigations, Dr. Reichlin helped to identify the limbic system as associated with both depression and sense of smell.6 Thus, Dr. Reichlin’s generosity and inquisitiveness “were instrumental in identifying the autoimmune mechanism responsible for psychiatric manifestations, and led to the new field that we later developed about smell and the autoimmune diseases,” says Dr. Shoenfeld.7
Dr. Reichlin has published more than 331 papers, lectured worldwide, and received a plethora of awards. His body of work, including his demonstration of the pathogenic roles of autoantibodies in SLE (anti-Ro in skin lesions and anti-Ro from affected kidneys), garnered him the Evelyn V. Hess, MD, Research Award, presented in 2006 at the ACR annual meeting. He also received a prize for lifetime contributions to autoimmunity from the International Congresses of Autoimmunity. Looking back on his productive career, Dr. Reichlin says, “It was always exciting to come into new areas that had not been explored before, and find a direction that was fruitful and productive.” Dr. James notes that Dr. Reichlin often emphasized that “things don’t always go perfectly in the lab—or the clinic—and that part of the work is persistence and perseverance and trying to do what’s best for the patients.”
Because of his dedication to patient-oriented research, tens of thousands of patients are helped by his discoveries every year. With characteristic modesty, Dr. Reichlin adds, “Finding ways around brick walls is what research is all about. I just wanted to solve problems and see where it led me. And it’s worked out very well.”
Gretchen Henkel is writing the “Profiles in Rheumatology” series.
Timeline
1959 – Earns MD from Washington University, St. Louis
1959 – Becomes intern at Bronx Municipal Hospital Center (Albert Einstein College of Medicine)
1960 – Becomes assistant resident at Bronx Municipal Hospital Center
1961 – Becomes research associate at Brandeis University
1963 – Begins postdoctoral fellowship at University of Rome
1964 – Becomes an instructor at University of Vermont College of Medicine
1965 – Becomes assistant professor of medicine at State University of New York at Buffalo School of Medicine
1968 – Becomes associate professor of medicine and biochemistry at State University of New York at Buffalo School of Medicine
1971 – Becomes professor of medicine and biochemistry at State University of New York at Buffalo School of Medicine
1974 – Completes a sabbatical at the Royal College of Surgeons in London
1981 – Becomes professor of medicine and chief of the immunology section at University of Oklahoma Health Sciences Center
1981 – Becomes head of the arthritis and immunology program at OMRF
References
- Clark, G, Reichlin, M, Tomasi, TB. Characterization of a soluble cytoplasmic antigen reactive with sera from patients with systemic lupus erythematosus. J Immunol. 1969. 102:117-122.
- Reichlin M, Hay M, Levine L. Immunochemical studies of hemoglobin and myoglobin and their globin moieties. Biochemistry. 1963;2:971 979.
- Reichlin M, Hay M, Levine L. Antibodies to human A1 hemoglobin and their reactions with A2, S, C and H hemoglobins. Immunochemistry. 1964;1:21 30.
- Reichlin M, Fogel S, Nisonoff A, Margoliash E. Antibodies against cytochromes c from vertebrates. J Biol Chem. 1966;241:251 253.
- Reichlin M. Use of antibody in the study of protein structure in protein sequence determination. In: Needleman SB, ed: Molecular Biology, Biochemistry and Biophysics, Vol. 25: Advanced Methods in Protein Sequence Determination. New York, NY: Springer Verlag; 1977:55 67.
- Katzav A, Solodeev I, Brodsky O, et al. Induction of autoimmune depression in mice by anti-ribosomal P antibodies via the limbic system. Arthritis Rheum. 2007;56:938-948.
- Katzav A, Ben-Ziv T, Chapman J, Blank M, Reichlin M, Shoenfeld Y. Anti-P ribosomal antibodies induce defect in smell capability in a model of CNS-SLE (depression). J Autoimmun. 2008;31:393-398.


