Medically Unlikely Edits (MUEs) were launched on January 1, 2007 by the Centers for Medicare and Medicaid Services (CMS) to reduce the paid claims error rate for Medicare Part B claims. The function of MUEs is to detect and deny unlikely CMS claims for a Medicare patient on a single, 24-hour date of service on a prepayment basis. This is achieved by limiting the frequency of services provided by a physician or medical supply company.
MUEs versus NCCI Edits
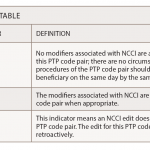
Although the CMS adheres to both MUEs and National Correct Coding Initiative (NCCI) Edits, the two are very different. MUEs are based on a single code and are limited by frequency within a date of service, while NCCI edits are comparing two codes that are billed at the same encounter and one is considered to be a component of the other procedure.
MUEs are edits that are based on anatomic, Current Procedural Terminology (CPT) code descriptions, CPT coding instructions, and medical reasonableness. These edits will test claims on the same beneficiary, Healthcare Common Procedure Code System, date of service, and the provider against a standard number of units of service. Examples of some of these edits are:
- The injection(s); single or multiple trigger point(s); three or more muscle(s) would be set at one.
- Ultrasound guidance placement for injections would be set at one per 24 hours per patient.
- Medical reasonableness would be set to the maximum number of a service that could be performed on a patient in a day.
Ultrasound Guidance
With the increase use of the ultrasound guidance, CPT code 76942 has been placed on the MUE list. One of the great uses of ultrasound guidance can be for needle placement for joint injections. If you use ultrasound guidance for needle placement, be aware that more Medicare carriers are enforcing the one ultrasound guidance per 24 hours per patient MUE. Please see this month’s Coding Corner on page 14 for an appropriate billing scenario.
Also keep in mind that it is not permissible to bill the patient for denied MUE or NCCI edits, even if there is a signed advance beneficiary notice (ABN) on file. This denial is not a medical necessity denial, but a coding denial. In an April 14, 2009 letter, the CMS stated that, “providers cannot utilize an ABN under any circumstances to bill a Medicare patient for service denied due to an MUE, even if the denial is upheld due to lack of medical necessity on appeal.”