WASHINGTON, D.C.—Often, no clear explanation exists in neutrophilic dermatosis cases that links a patient’s skin disorder with an internal condition, expert Joseph Jorizzo, MD, professor, founder and former chair of the Dermatology Department at Wake Forest University in Winston-Salem, N.C., and professor of clinical dermatology at Wevascularill Cornell Medical College in New York, told attendees in the 2016 ACR/ARHP Annual Meeting session titled, Neutrophilic Dermatoses.
Neutrophilic Vascular Reactions
“One of the things I want to really highlight,” Dr. Jorizzo said, “is the difference between the kind of dermatoses where a clinical pathologic diagnosis ties together the patient’s internal complaints and their cutaneous findings, such as sarcoidosis or lupus or dermatomyositis, and focus on a prime category of reactive dermatoses.”
About half of patients in the “reactive” category will have no underlying disease, he said. The others may have a process that is caused by a reaction to a rheumatologic, gastroenterologic or myelodysplastic condition, or some other disorder.
“So [reactive diseases] require even more teamwork among colleagues than do the other diseases, where you just walk in, and the skin and inside is all together,” Dr. Jorizzo said.
These diseases, described as “neutrophilic vascular reactions” in a 1988 paper led by Dr. Jorizzo, include Sweet’s syndrome, Behçet’s disease, bowel-associated dermatosis-arthritis syndrome and pyoderma gangrenosum.1
“I like to include the word vascular, because I believe the neutrophilic process is vessel based, primarily, and that distinguishes this from diseases where the epidermis is the target, such as psoriasis,” Dr. Jorizzo said.
The biopsy is a crucial element in the diagnosis of these diseases, but getting one that’s actually helpful is not a simple proposition, he added.
“There’s a certain art in delivering to the pathologist [that which] gives you a chance of getting the diagnosis,” he said. “You want a lesion that’s just far enough advanced to have the classic changes, but not so far advanced that those changes are masked by secondary change.”
He also emphasized the concept of a therapeutic ladder—that the intensity of a therapy and the risk that’s willing to be tolerated—should be capped based on the extent of the disease.
Sweet’s Syndrome
Sweet’s syndrome involves fever and malaise, along with erythematous plaques on clinical exam. Histologically, its traits include dense perivascular neutrophilic leukocytoclasia with minimal, or even no, evidence of vasculitis. Associated conditions can include infections, malignancies, inflammatory bowel disease and autoimmune disorders.
Dr. Jorizzo said thalidomide is often his preferred treatment for Sweet’s syndrome. This prescribed treatment can sometimes cause difficulties with health insurance companies because they might want an oncologist to approve the medication. Dr. Jorizzo mentioned a patient with whom this was the case. When the oncologist balked at the request, he sent the patient to him with a severe case of Sweet’s on the face, at which point the oncologist signed off right away.
Behçet’s Disease
Behçet’s is a multisystem disease with many symptoms. Skin findings range from sterile papulopustules and palpable purpura to erythema nodosum-like lesions. On histology, a neutrophilic infiltrate will be seen, with leukocytoclastic vasculitis early in the disease course and lymphocytic vasculitis late in the course.
Dr. Jorizzo said he is struck by how often Behçet’s disease is overdiagnosed. The problem, he said, is that many people have canker sores, many have genital herpes and nearly everyone has acne. If you add in an issue with the eye, nearly all of the criteria for this diagnosis are then met, he said.
In 2005, Dr. Jorizzo documented how out of 81 patients referred to his clinic with Behçet’s, only 10 of them actually had the disease.2 Fifty-four of them had complex aphthosis, another disorder which is characterized by ulcers, but is much less serious.
‘I like to include the word vascular, because I believe the neutrophilic process is vessel based, primarily, & that distinguishes this from diseases where the epidermis is the target, such as psoriasis.’ —Dr. Jorizzo
Bowel-Associated Dermatosis-Arthritis Syndrome
Speaking about bowel-associated dermatosis-arthritis syndrome, Dr. Jorizzo described it as a condition similar to a syndrome that used to be seen in patients who’d had bowel bypass surgery. Even after that procedure was discontinued, there were still patients with erythematous and purpuric papules and vesicles and nodular panniculitis, with associated polyarthritis and tenosynovitis.
Findings on histopathology include dermal nodular perivascular neutrophilic infiltrate with edema and lobular neutrophilic and septal panniculitis. Dr. Jorizzo said he described this condition many years ago in a previous study.3
He said that inflammatory bowel diseases are important causes and emphasized management of the underlying disease.
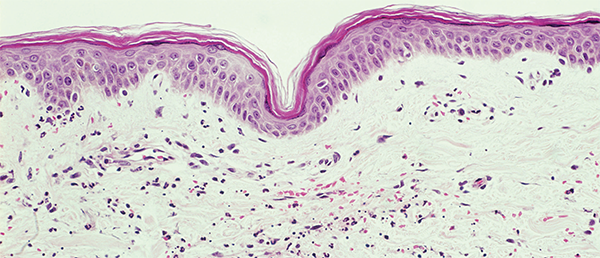
Small vessel neutrophilic vasculitis.
Biophoto Associates/ScienceSource.com
Pyoderma Gangrenosum
On the topic of pyoderma gangrenosum, Dr. Jorizzo said this condition can appear with ulcers, be bullous, involve pustules or appear in a superficial granulomatous form. The most characteristic lesion, Dr. Jorizzo said, is an ulcer with a necrotic undermined border and a base that can be purulent or vegetative.
Most patients with pyoderma gangrenosum have large ulcers, he said, but no inflammation. One way to tell that there is no inflammation—and that the patient only needs wound healing—is the “Gulliver’s sign,” rope-like strands of epithelium crossing from the skin to the bed of the ulcer, he added.
He said this is a diagnosis of exclusion and that it’s important to look for mimics, including granulomatosis with polyangiitis histoplasmosis. He said he’s even been surprised by the how frequently he sees factitial disease, in which people harm their own skin.
“You would be amazed,” Dr. Jorizzo said, “at what people do to legitimize a psychiatric problem with a medical one.”
Thomas R. Collins is a freelance writer living in South Florida.
References
- Jorizzo JL, Solomon AR, Zanolli MD, et al. Neutrophilic vascular reactions. J Am Acad Dermatol. 1988 Dec;19(6):983–1005.
- Letsinger JA, McCarty MA, Jorizzo JL. Complex aphthosis: A large case series with evaluation algorithm and therapeutic ladder from topicals to thalidomide. J Am Acad Dermatol. 2005 Mar;52(3 Pt 1):500–508.
- Jorizzo JL, Apisarnthanarax P, Subrt P, et al. Bowel-bypass syndrome without bowel bypass. Bowel-associated dermatosis-arthritis syndrome. Arch Intern Med. 1983 Mar;143(3):457–461.


