Both PM and DM present subacutely over weeks to months with proximal muscle weakness. The photosensitive skin manifestations of DM include facial erythroderma without sparing of the nasolabial folds that is typical in lupus erythematosus; heliotrope rash around the eyes; Gottron’s rash/papules (see Figure 2, below); and shawl and v-neck signs. Patients with MSAs can be categorized by typical features associated with these antibodies. See Table 3 (p. 22) for a list of features associated with particular autoantibodies.
In contrast to the presentation of PM and DM, the onset and progression of IBM is characteristically slow, occurring over months to years. Asymmetric weakness, dysphagia, frequent falling, and distal as well as proximal muscle weakness and wasting are hallmarks of this IIM subset.
IIM can present in overlap with other rheumatic diseases, including systemic lupus erythematosus, progressive systemic sclerosis (scleroderma), Sjögren’s syndrome, and RA. The onset of myositis symptoms can occur at, before, or after diagnosis of these diseases. Overlap with IBM is far less common, but has been reported.
The association of IIM with malignancy is well recognized. In a review of four studies comprising 1,078 myositis patients and a comparable number of controls, the overall odds ratio (OR) for the association of cancer with DM was 4.4 (95%, confidence interval [CI] 3.0, 6.6) and with PM the OR was 2.1 (95% CI 1.4, 3.3).6 Malignancies are predominantly adenocarcinomas and usually develop within one year before or after myositis onset, but have been reported to occur up to five years later.7 Therefore, age-appropriate cancer screening and ongoing surveillance with a lowered threshold for further investigation is mandated.
Approximately 30% of DM cases present without clinically apparent muscle weakness, the majority of which progress months or years later to clinical myositis.8 Patients without evidence of muscle weakness or serum muscle enzyme abnormalities are classified as dermatomyositis sine myositis or amyopathic DM. These patients can develop interstitial lung disease (ILD) which can be rapidly progressive, heralding a poor prognosis.9,10
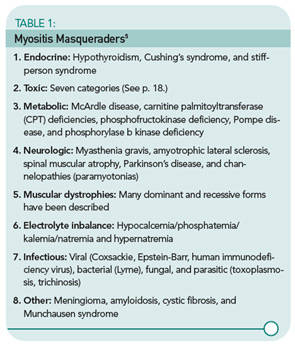
The importance of evaluation for toxic myopathies cannot be stressed enough, for as a group toxins represent the most common etiology of myopathy. In an elegant review of this topic, Walsh and Amato classified the toxic myopathies to date according to presumed pathogenic mechanism into seven categories:11
- Necrotizing myopathy: Alcohol, anti-lipemic agents (statins and fibrates), cyclosporin, labetolol, propofol, illicit drugs (cocaine, heroin, amphetamines), and controlled substances (meperidine, pentazocine);
- Amphiphilic: Amiodarone, chloroquine, and hydroxychloroquine;
- Antimicrotubular: Colchicine and vincristine;
- Mitochondrial myopathy: Zidovudine;
- Inflammatory myopathy: L-tryptophan, D-penicillamine, cimetidine, L-dopa, phenytoin, lamotrigine, interferon-α, hydroxyurea, and imatinib;
- Hypokalemic myopathy: Diuretics, laxatives, amphotericin, toluene abuse, licorice, corticosteroids, and alcohol abuse; and
- Unknown: Critical illness myopathy (corticosteroids, nondepolarizing neuromuscular blocking agents, and sepsis), omeprazole, isoretinoin, finasteride, and emetine.
Obtaining a family history of similar symptoms and neuromuscular disease is important; a positive response is most likely indicative of pathology other than IIM, such as in the muscular dystrophy in the case study above. A notable exception is IBM, because both idiopathic and familial forms exist.
Laboratory Tests
Muscle enzymes: As noted above, elevations of serum concentration of intracellular muscle components (CK, aldolase, AST, ALT, LDH, and myoglobin) generally accompany myositis. In IBM, serum CK correlates poorly with disease acuity and severity. It is normal in 25% of patients and, if abnormal, it is generally only slightly elevated.12

Tests commonly called “liver function tests” actually test for liver-associated enzymes such as AST, ALT, and LDH—which are also found in muscle. Unfortunately, it is common for patients to present to rheumatologists after a liver biopsy is performed due to elevated “liver function tests” resulting from active myositis. In this case, the liver biopsy is normal. Also remember that, when monitoring a patient with active myositis and elevated CK being treated with MTX, increased AST and ALT are more likely to reflect active disease than MTX-induced hepatic toxicity.