Tashatuvango / shutterstock.com
The idiopathic inflammatory myopathies (IIM) encompass eight categories: 1) dermatomyositis (DM) in adults, 2) juvenile dermatomyositis, 3) amyopathic DM, 4) cancer-associated DM, 5) polymyositis, 6) immune-mediated necrotizing myopathy, 7) inclusion body myositis, and 8) overlap myositis.1 These categories help classify the myopathies based on clinical and histologic features. The incidence of IIM is estimated at 2–15 new cases per year per million inhabitants, depending on country, with a peak range of onset in adults between 45 and 60 years old.1,2
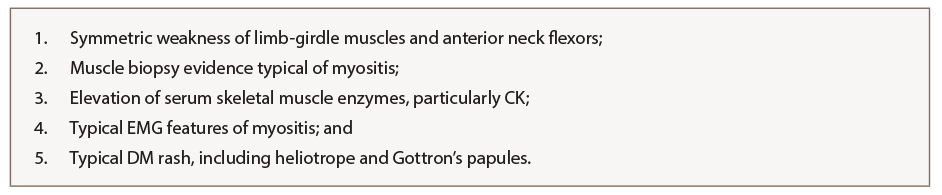
One of the most widely used classification criteria for myositis was described by Bohan and Peter in 1975.3 Depending on the number of criteria fulfilled, a diagnosis of polymyositis or dermatomyositis can be made. These criteria incorporate clinical features of weakness, histopathologic evidence on muscle biopsy, elevation of skeletal muscle enzymes, features on electromyogram (EMG) and cutaneous manifestations (see Table 1). Importantly, use of these criteria first requires exclusion of other potential myopathies, including muscular dystrophy; neurologic disease, including myasthenia gravis; metabolic or endocrine myopathies; and infectious myositis.
Reclassification of Inflammatory Myopathies
Since 1975, various attempts at reclassification of inflammatory myopathies have incorporated inclusion body myositis and immune-mediated necrotizing myopathy, once these entities were recognized. In 2004, the International Myositis Classification Criteria Project was established, which included experts across multiple adult and pediatric subspecialties (i.e., rheumatology, neurology, dermatology). The project involved collecting data between 2008 and 2011 from more than 975 patients with IIM (75% adults and 25% children), with 624 having mimicker conditions, or non-IIM. Statistical models helped identify 16 variables from six different categories that were helpful in distinguishing IIM from mimicking comparators.
Based on statistical results, a scoring system was created in which points are added to yield a probability of having IIM. The scoring system incorporates cutaneous manifestations; laboratory measurements, such as muscle enzymes and presence of anti-Jo-1 autoantibodies; clinical manifestations; and muscle biopsy features. With muscle biopsy, the 2017 European League Against Rheumatism (EULAR)/ACR classification criteria have much improved sensitivity (93%) and specificity (88%) over prior classification criteria.4 Once a patient first meets EULAR/ACR classification criteria for IIM (probability ≥55%), a classification tree for subgroups of IIM was developed (see Figure 1, and Table 2) to further subclassify the patient. An online calculator IIM is available to help clinicians use the new classification criteria.