These same findings of hyperalgesia and allodynia have been noted in most of the other conditions acknowledged to be part of this continuum, including irritable bowel syndrome (IBS), temporomandibular joint disorder, tension type headache, idiopathic low back pain, vulvodynia, and interstitial cystitis.19-25
Brain imaging studies also demonstrate the existence of central pain augmentation in FM, IBS, low back pain, and several other central sensitivity syndromes (CSSs).26-29
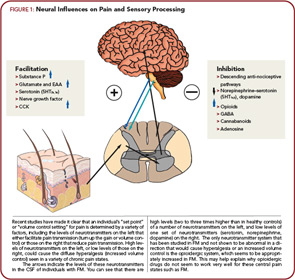
The Role of Specific Neurotransmitters
Rheumatologists might best understand pain and sensory processing by considering that this type of processing is controlled in a manner very similar to immune function. Just as high levels of proinflammatory cytokines, or low levels of antiinflammatory cytokines, can move an individual towards hyperimmune function, there are neurotransmitters that are similarly known to either increase or decrease pain transmission in the central nervous system (CNS). Overall, the analogy of an increased “volume control” or “gain” setting on pain and sensory processing is supported by studies from a variety of sources. Similar to essential hypertension, where a variety of root causes can lead to elevated systemic blood pressure, these disorders represent essential hypertension of pain and sensory processing pathways. Elevated levels of neurotransmitters that tend to be pro-nociceptive (see the left side of Figure 1, above) or reduced levels of neurotransmitters that inhibit pain transmission (see the right side of Figure 1) have a tendency to increase the volume control, and drugs that block neurotransmitters on the left or augment activity of those on the right will typically be effective treatments, at least for a subset of individuals with this spectrum of illness.