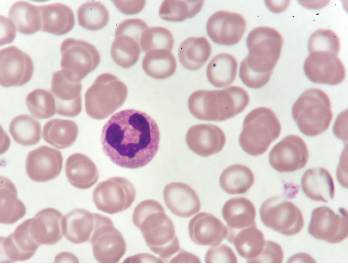
A neutrophil in a blood smear.
Jarun Ontakrai / shutterstock.com
Certain medications have been associated for decades with the development of drug-induced autoimmunity. New research published in March 2018 in Arthritis & Rheumatology suggests that NETs (neutrophil extracellular traps) are potentially implicated in the mechanisms that lead to drug-induced autoimmunity.1
Peter Grayson, MD, MSc, head of the Vasculitis Translational Research Program at the National Institute of Arthritis and Musculoskeletal and Skin Diseases, says that research related to NETs may have no current clinical implications, but he predicts that research focused on NETs “is likely to unlock novel therapeutic strategies in a range of rheumatologic diseases.” Understanding the role of NETs in drug-induced autoimmunity may be the next step toward clarifying the mechanisms of autoimmunity.
NET formation is involved in the neutrophil cell death process, called NETosis, which is different morphologically from other types of cell death, including apoptosis and necrosis. In NETosis, the dying neutrophils “can unwind their DNA and launch it out of the cell like a spiderweb to engulf and facilitate the elimination of pathogens,” Dr. Grayson explains. The process, however, can become aberrant in many rheumatologic diseases with the dysregulation of NET formation.
“What is surprising and potentially interesting for rheumatologists to understand is that there is only a small number of proteins inside these NETs, and many of them are the antigenic targets of autoantibodies in rheumatologic diseases,” Dr. Grayson says. Patients with rheumatoid arthritis make anticyclic citrullinated peptide (CCP) antibodies directed to proteins found in the NETs. Patients with lupus make antibodies to NET components. Proteinase 3 and myeloperoxidase, the antigenic targets of antineutrophil cytoplasmic antibodies (ANCA) are commonly found within NETs.
“These proteins that are normally hidden inside a neutrophil get exposed to the adaptive immune system in a way that is immunogenic, which then can potentially lead to development of antibodies to those proteins,” says Dr. Grayson.
NET formation and impaired NET degradation have been implicated in the pathogenesis of both systemic lupus erythematosus (SLE) and ANCA-associated vasculitis (AAV). “The process of NETosis may contribute to causal mechanisms of disease in rheumatoid arthritis, lupus and AAV,” he says.
In NETosis, the dying neutrophils ‘can unwind their DNA & launch it out of the cell like a spiderweb to engulf & facilitate the elimination of pathogens,’ Dr. Grayson explains.
Triggering NET Formation, Degradation
Previous research that examined drug-induced autoimmunity looked at the effect of medications on lymphocytes. This new research by Dr. Grayson and colleagues looked at their effect on neutrophils and NETs. Medications associated with drug-induced autoimmunity can lead to development of a rheumatologic disease that “has a specific look or feel to it. It looks a lot like lupus mixed with ANCA vasculitis. We thought that because NETs are important in lupus and ANCA vasculitis, maybe the drugs are inducing NETs, since it’s a common theme to those conditions,” Dr. Grayson explains.
Certain medications associated with drug-induced autoimmunity were previously shown to trigger NET formation and to impair NET degradation. The thyroid medication propylthiouracil, linked to drug-induced AAV, can induce NET formation and impair NET degradation.2 Also, cocaine that has been contaminated with levamisole, an antihelmintic drug, can induce NETs, doing so through cholinergic receptors, Dr. Grayson says.3
For this study, researchers examined the effect of four medications causally linked to drug-induced autoimmunity—procainamide, hydralazine, minocycline and clozapine—on NET formation, NET degradation and NET protein content. The rationale of the research was to demonstrate that some drugs linked with drug-induced autoimmunity enhance NET formation. These findings could then potentially provide evidence that neutrophils and NETs “are involved in the pathogenesis of specific drug-induced and idiopathic autoimmune diseases,” according to the published report.
In the study, neutrophils were first isolated from heparinized blood, and then the neutrophils were treated with the four drugs. After four hours of stimulation, procainamide and hydralazine induced significant NET formation, whereas the NET formation induced by clozapine and minocycline was not significant.
“This provides some indirect evidence that neutrophils are implicated in drug-induced autoimmunity and that the drugs may trigger NETs as a potential inciting event in why these patients develop autoantibodies,” Dr. Grayson says. “One of the hallmarks of drug-induced autoimmunity is that these patients usually develop multiple different antibodies, so the same patient can make an antibody seen in lupus and ANCA vasculitis at the same time.”
The research also provides new information about the signaling pathways by which the drugs trigger NETs. According to Dr. Grayson, hydralazine triggers NETs by altering intracellular calcium levels in neutrophils. Procainamide, which is no longer used in clinical practice, triggers NETs by binding to cholinergic receptors on the surface of neutrophils. “That suggests that there is crosstalk between neutrophils, or innate immune cells, and the autonomic nervous system transmitters.”
The results indicate the class of drugs that could potentially triggers NETs. “We would predict that drugs that basically bind and modulate cholinergic receptors would be more likely to trigger NETs, and similarly, drugs that modulate intracellular calcium levels could also potentially trigger NETs,” Dr. Grayson says. The onset of autoimmunity by a hydralazine or similar drug will not necessarily occur when the patient first starts taking it. In fact, it can happen months or years later, he says.
Drug-Induced Autoimmunity: A Disease Model
Drug-induced autoimmunity is providing an “excellent disease model to further understand idiopathic disease,” according to an editorial published with the research report.4 “Additional exploration and characterization of drug-induced NETosis and the autoantigen ‘cargo’ carried within released NETs will help us better understand autoimmune mechanisms,” Amr H. Sawalha, MD, at the University of Michigan, Ann Arbor, wrote in his editorial.
Drug-induced autoimmunity is not as complex a disease as lupus or ANCA vasculitis because there is a known trigger that can be turned on or turned off. “The rationale underlying this work is that we can learn and study drug-induced autoimmunity, which is a simpler condition, and then apply what we learn to the more complex [conditions],” Dr. Grayson says.
One potential outcome of research into NET formation and its relationship with lupus and ANCA vasculitis and autoimmunity is that future drug development could focus on blocking NET formation as a new therapeutic target for this family of diseases. Although it is disconcerting to think of targeting neutrophils therapeutically because they fight infection, “we may eventually be able to target a specific process within neutrophils that is causing disease, and then we could be a little more selective in treatment,” Dr. Grayson says.
Medications commonly used in rheumatologic diseases often target lymphocytes and the adaptive immune system. Targeting neutrophils and the innate immune system may more directly target causal factors in certain diseases, he explains.
The evidence right now is “a bit circumstantial until we can put these into animal models and can start blocking these processes in humans. However, there is a mounting body of evidence beyond just this paper suggesting that we are on the right track,” Dr. Grayson says.
Kathy Holliman, MEd, has been a medical writer and editor since 1997.
References
- Irizarry-Caro JA, Carmona-Rivera C, Schwartz DM, et al. Drugs implicated in systemic autoimmunity modulate neutrophil extracellular trap formation. Arthritis Rheumatol. 2018 Mar;70(3):468–474.
- Nakazawa D, Tomaru U, Suzuki A, et al. Abnormal conformation and impaired degradation of propylthiouracil-induced neutrophil extracellular traps: Implications of disordered neutrophil extracellular traps in a rat model of myeloperoxidase antineutrophil cytoplasmic antibody–associated vasculitis. Arthritis Rheum. 2012 Nov;64(11):3779–3787.
- Carmona-Rivera C, Purmalek MM, Moore E. A role for muscarinic receptors in neutrophil extracellular trap formation and levamisole-induced autoimmunity. JCI Insight. 2017 Feb 9;2(3):e89780.
- Sawalha AH. Editorial: The innate and adaptive immune response are both involved in drug-induced autoimmunity. Arthritis Rheumatol. 2018 Mar;70(3):330–333.


