Rheumatologists are likely to follow a conservative path in their choices, and study results have to be applied to real-life situations. “The treatments that studies suggest are more effective, we know they come with a slightly higher risk of side effects and higher costs. But the cost picture is also changing,” he added, as the manufacture of biologic agents becomes more effective.
“I don’t think we can say any more that the reason we’re not choosing some of these newer therapies is because they’re too new. But we can say we feel there are certain advantages and disadvantages to these drugs, and also to conventional treatments—and we need to balance those considerations. We also need to be honest and say that, right now, cost is a factor in our decisions.” European and American guidelines are not yet recommending that RA patients be treated with biologics as a first-line treatment, he noted.
“But we’re seeing the contours of new treatments that will be more cost-effective,” for example, induction-maintenance therapies and the use of Janus kinase (JAK) inhibitors or other powerful treatments early on, for a limited time, to bring the disease under control as quickly and effectively as possible. “Then you build on it by giving maintenance therapy.” JAK inhibitors, including tofacitinib and baricitinib, target a family of intracellular Tyrosine kinases that transduce cytokine-mediated signals in the cells.
Currently, there are nine originator biologicals approved by the FDA for treating RA, plus one biosimilar, although three biosimilars for RA are used in Europe. Collectively, they have five distinct mechanisms of action, and more are in the pipeline, Dr. van Vollenhoven said.1,2
Other new strategies highlighted in his presentation include neuroimmunomodulation of the inflammatory response, which has been tested in the form of an implantable device in the neck to stimulate the vagal nerve.3 “It’s a complicated procedure, but some patients did well on it,” he said.
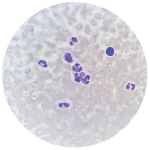
Fluorescent optical imaging can be used to detect subclinical synovitis, an inflammation of the joint lining, a primary characteristic of inflammatory arthritis, according to a study published last year.4 Ultrasound can also help support diagnostics. A multi-biomarker disease activity (MBDA) score procedure has been approved by the Food and Drug Administration to show level of disease activity.
In a new study at Karolinska in Sweden, it was found that for patients who have clinically active disease but a low MBDA, triple therapy may be better than anti-tumor necrosis factor, he said.
Clearly, one dose does not fit all with RA, & there is a balancing act involving treatment advances. —Dr. van Vollenhoven
Personalized Care
“Doesn’t it strike you as odd that all patients get the same dose of these new drugs, whether they are large or small?” Dr. van Vollenhoven asked. “What would a personalized dose offer? Dosages based on clinical trials give you an average approach, but once a drug is approved, the manufacturer doesn’t have a motivation to keep studying different dosages.”