For recurrent acute arthritis and refractory chronic arthritis, there are possible benefits, described in small, inadequately controlled studies of hydroxychloroquine (presumably by decreasing phagolysosomal-mediated crystal-induced NLRP3 inflammasome activation) and methotrexate.15,19 Conversely, rebound arthritis after tapering systemic corticosteroids could be an issue mediated by the known ability of corticosteroids to induce NLRP3 production in macrophages. There is no clear benefit of anti–tumor necrosis factor (TNF) therapy in CPPD. However, interleukin 1 antagonism clearly merits further investigation for refractory CPPD arthritis, as in gout.20
It is not yet clear whether oral magnesium supplementation will have benefits in inhibiting crystal deposition in established CPPD.15 For example, promotion of crystal dissolution by recombinant alkaline phosphatase risks flares of acute arthritis by crystal shedding from cartilage.15 ENPP1 activity, and ANKH transport function (which is nonselectively inhibited by probenecid) represent compelling targets for future molecular therapeutics to suppress crystal deposition in severe, symptomatic CPPD.15
Conclusion
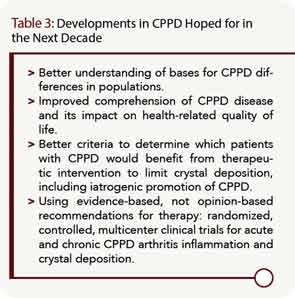
Writer Hugh Prather described life as “a mixture of unsolved problems, ambiguous victories, and vague defeats with very few moments of clear peace.” So it is metaphorically in rheumatology, at present, with CPPD. The last decade has seen substantial advances in the disorder, but huge hurdles remain (see Table 3). A good starting point would be a multicenter, randomized, controlled clinical trial of symptomatic disease subsets driven by CPPD.
Acknowledgment
This work was supported by the Veteran’s Affairs Research Service and the National Institutes of Health grant PAG07996. Dr. Terkeltaub is a consultant to Takeda Pharmaceutical Company Ltd., Pfizer Inc., Regeneron Pharmaceuticals Inc., and Novartis Pharmaceuticals.
Dr. Terkeltaub is chief of the rheumatology section at the Veterans Affairs Medical Center in San Diego, and a professor of medicine at the University of California, San Diego School of Medicine.
References
- Abhishek A, Doherty S, Maciewicz R, Muir K, Zhang W, Doherty M. Chondrocalcinosis is common in the absence of knee involvement. Arthritis Res Ther. 2012;14:R205.
- Abhishek A, Doherty S, Maciewicz R, Muir K, Zhang W, Doherty M. Evidence of a systemic predisposition to chondrocalcinosis and association between chondrocalcinosis and osteoarthritis at distant joints: A cross-sectional study. Arthritis Care Res (Hoboken). 2013;65:1052-1058.
- Zhang Y, Terkeltaub R, Nevitt M, et al. Lower prevalence of chondrocalcinosis in Chinese subjects in Beijing than in white subjects in the United States: The Beijing osteoarthritis study. Arthritis Rheum. 2006;54:3508-3512.
- Johnson K, Jung A, Murphy A, Andreyev A, Dykens J, Terkeltaub R. Mitochondrial oxidative phosphorylation is a downstream regulator of nitric oxide effects on chondrocyte matrix synthesis and mineralization. Arthritis Rheum. 2000;43:1560-1570.
- Johnson K, Svensson CI, Etten DV, et al. Mediation of spontaneous knee osteoarthritis by progressive chondrocyte ATP depletion in Hartley guinea pigs. Arthritis Rheum. 2004;50:1216-1225.
- Rho YH, Zhu Y, Zhang Y, Reginato AM, Choi HK. Risk factors for pseudogout in the general population. Rheumatology (Oxford). 2012;51:2070-2074.
- Abhishek A, Doherty M. Pathophysiology of articular chondrocalcinosis—role of ANKH. Nat Rev Rheumatol. 2011;7:96-104.
- Terkeltaub R, Pritzker KPH. Pathogenesis and molecular genetics of calcium pyrophosphate dihydrate crystal deposition disease. In: Terkeltaub R, ed. Gout and Other Crystal Deposition Arthropathies. Philadelphia, Penn: Elsevier; 2011:240-248.
- Costello JC, Rosenthal AK, Kurup IV, Masuda I, Medhora M, Ryan LM. Parallel regulation of extracellular ATP and inorganic pyrophosphate: Roles of growth factors, transduction modulators, and ANK. Connect Tissue Res. 2011;52:139-146.
- Johnson K, Farley D, Hu SI, Terkeltaub R. One of two chondrocyte-expressed isoforms of cartilage intermediate-layer protein functions as an insulin-like growth factor 1 antagonist. Arthritis Rheum. 2003;48:1302-1314.
- Jubeck B, Muth E, Gohr CM, Rosenthal AK. Type II collagen levels correlate with mineralization by articular cartilage vesicles. Arthritis Rheum. 2009;60:2741-2746.
- Martinon F, Pétrilli V, Mayor A, Tardivel A, Tschopp J. Gout-associated uric acid crystals activate the NALP3 inflammasome. Nature. 2006;440:237-241.
- Zhang Y, Johnson K, Russell RG, et al. Association of sporadic chondrocalcinosis with a -4-basepair G-to-A transition in the 5’-untranslated region of ANKH that promotes enhanced expression of ANKH protein and excess generation of extracellular inorganic pyrophosphate. Arthritis Rheum. 2005;52:1110-1117.
- Zhang W, Doherty M, Bardin T, et al. European League Against Rheumatism recommendations for calcium pyrophosphate deposition. Part I: Terminology and diagnosis. Ann Rheum Dis. 2011;70:563-570.
- Guerne PA, Terkeltaub R. Calcium pyrophosphate dihydrate crystal deposition: Epidemiology, clinical features, diagnosis, and treatment. In: Terkeltaub R, ed. Gout and Other Crystal Deposition Arthropathies. Philadelphia, Penn: Elsevier; 2011:249-265.
- Neogi T, Nevitt M, Niu J, et al. Lack of association between chondrocalcinosis and increased risk of cartilage loss in knees with osteoarthritis: Results of two prospective longitudinal magnetic resonance imaging studies. Arthritis Rheum. 2006;54:1822-1828.
- Frediani B, Filippou G, Falsetti P, et al. Diagnosis of calcium pyrophosphate dihydrate crystal deposition disease: Ultrasonographic criteria proposed. Ann Rheum Dis. 2005;64:638-640.
- Zhang W, Doherty M, Pascual E, et al. EULAR recommendations for calcium pyrophosphate deposition. Part II: Management. Ann Rheum Dis. 2011;70:571-575.
- Chollet-Janin A, Finckh A, Dudler J, Guerne PA. Methotrexate as an alternative therapy for chronic calcium pyrophosphate deposition disease: An exploratory analysis. Arthritis Rheum. 2007;56:688-692.
- Announ N, Palmer G, Guerne PA, Gabay C. Anakinra is a possible alternative in the treatment and prevention of acute attacks of pseudogout in end-stage renal failure. Joint Bone Spine. 2009;76:424-426.