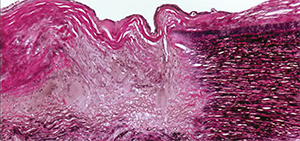
This photomicrograph of the aorta shows transmural destruction on the left side of the specimen with an inflammatory process containing multinucleated giant cells and loss of elastic fibers (Verhoeff-van Gieson stain).
ACR image library
LONDON—New therapies are emerging for the two main forms of large-vessel vasculitis, giant cell arteritis (GCA) and Takayasu’s arteritis—particularly biologic therapies. But for just about every available treatment gap, drawbacks or limited evidence remain, with the results needing to be borne out in larger trials, an expert said at the Annual Congress of the European League Against Rheumatism (EULAR) 2016.
It’s easy to see the need for better options, said Kenneth Warrington, MD, professor of medicine at the Mayo Clinic.
In GCA, glucocorticoids can help with symptoms and inflammatory markers, but those benefits come with vascular complications and even adverse effects, such as increased infection risk and sometimes pneumocystis pneumonia. Plus, relapses are common.1 GCA involves both the TH17 and TH1 pathway, but only one of these is addressed with glucocorticoids.
“Glucocorticoids very effectively abrogate the IL-17 pathway,” he said. “However, they leave the TH1 interferon gamma pathway essentially unchecked and this may lead to chronic smoldering vasculitides that may result in the clinical relapse that we see in our patients. This underscores the importance of more targeted and better therapy for these diseases.”
Similar effects—and problems—are seen with glucocorticoid use in Takayasu’s, he said.
Researchers have found mixed results in trials of methotrexate in GCA, with modest effects in reducing the risk of relapse and a reduction in steroid exposure, Dr. Warrington said.
Data on methotrexate and other conventional immunosuppressive agents in Takayasu’s are particularly thin, coming from a few open-label trials with fewer than 20 subjects per trial, but they show a good initial response followed by frequent relapses and disease progression. Dr. Warrington said that, since patients were also on glucocorticoids, it’s hard to know which therapy was exerting which effects.
Randomized controlled trials have found that TNF inhibitors don’t appear to be effective in GCA.
There is limited evidence that they work in Takayasu’s. One retrospective, multi-center study with 49 patients found a response in 83%, with adverse events in 16%—mostly infections, with two cancer cases.2
And, Dr. Warrington said, “despite the enthusiasm with these drugs, relapses are still seen in about a third.” The field still needs prospective trials on this, he said.
In both GCA and Takayasu’s, responses on IL-6-inhibitors have been seen in about 80% of patients, but with adverse events, including neutropenia and infection, seen in one out of four or five patients, Dr. Warrington said. Use of these therapies also appears to lower glucocorticoid use. And once treatment is ended, relapse is common, he said.

