It’s no secret that there will likely be a shortage of rheumatologists in the United States in the coming years. However, that may start to change once the subspecialty match dates for fellowships move, which will be effective for fellows starting in July 2013.
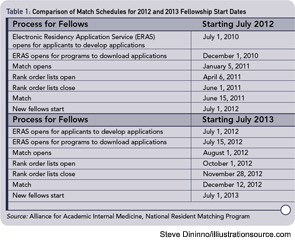
The date changes give residents applying for fellowships additional time to explore potential subspecialties and apply for fellowships. Beginning with students applying for July 2013 fellowships, the application process will start July 1, 2012, which will be most applicants’ post-graduate year 3 (PGY-3). Under the current system, residents begin subspecialty and fellowship choices and applications during PGY-2 (see Table 1 for the full schedule). With the new dates, fellowships usually will start six months after a match has been made, versus 18 to 20 months under the current system. Also, with the new dates, residents will have the chance to participate in approximately 10 rotations within various subspecialties.
The change in timing was prompted as early as 10 years ago by concerns from residency program directors that residents were not always sure which subspecialty they wanted to pursue, says Anne R. Bass, MD, associate professor of clinical medicine at Weill Cornell Medical College and rheumatology fellowship program director at the Hospital for Special Surgery in New York City. Dr. Bass is a member of the ACR Workforce and Training Committee who attended meetings regarding the Subspecialty Match date changes.
“A fair percentage of people make up their mind in residency regarding their subspecialty,” says Sharon Kolasinski, MD, associate professor of clinical medicine, interim division chief, chief of clinical services, and director of the rheumatology fellowship program at the University of Pennsylvania School of Medicine in Philadelphia. Dr. Kolasinski was lead author of a study asking rheumatology fellows why they chose rheumatology.1 “If there is no exposure to rheumatology in that time, they are unlikely to get it in their internship year, when there is a pretty inflexible curriculum.”
Additionally, the letters of recommendation written for fellowship applicants do not always contain enough valuable information because faculty may not have known students for that long a time, Dr. Bass says. Internships often expose students to intensive care, oncology, and other fields, while exposure to fields with rarer diseases is less common, Dr. Bass says. “A case of bad lupus is not seen as often as a myocardial infarction,” she says. By expanding the time that applicants have to select their subspecialty, there is a chance to expose a wider scope of students to rheumatology.


