Systemic lupus erythematosus (SLE) is a complex disease for clinicians and their patients, made even more challenging by health disparities that leave some patients with poorer outcomes. Since 2020, the ACR has been leading a project to reduce inequities in symptom recognition, care and disease management of SLE. The project is funded through a five-year grant from the Centers for Disease Control and Prevention (CDC).
One goal of the project is to develop and implement quality measures for patients diagnosed with lupus. This includes developing electronic health record (EHR) tools and utilizing the ACR’s Rheumatology Informatics System for Effectiveness (RISE) registry to provide the data most useful to both rheumatologists who care for patients with lupus and researchers conducting SLE studies.1

Dr. Bartels
Toward this end, the ACR formed two work groups to identify and address measure gaps. One is focused on longitudinal quality measures and is led by project co-lead Christie Bartels, MD, MS, division chief of rheumatology and associate professor of rheumatology, University of Wisconsin School of Medicine and Public Health, Madison, who is working with April Jorge, MD, assistant professor of medicine, Harvard Medical School, Boston, and director of the lupus program in the Division of Rheumatology, Allergy & Immunology at Massachusetts General Hospital, Boston. The second work group is focused on patient-reported outcome (PRO) measures and is led by project co-lead Jinoos Yazdany, MD, MPH, professor of rheumatology, Department of Medicine, University of California San Francisco (UCSF), and chief of rheumatology at San Francisco General Hospital, who is working with Patricia Katz, PhD, professor emerita of medicine and health policy, UCSF.

Dr. Yazdany
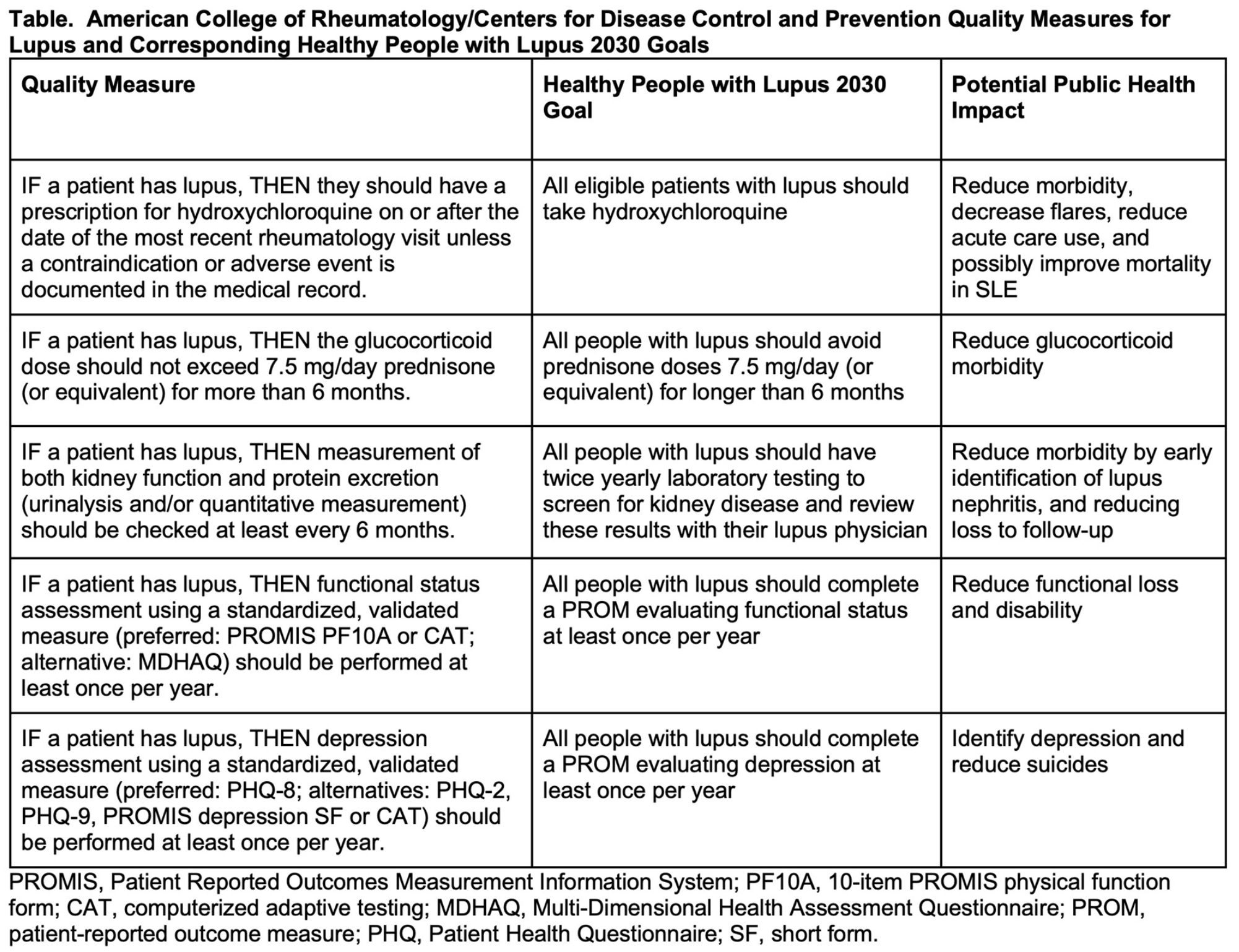
Now in the fourth year of the grant, the work groups have already had significant achievements. They have identified three across-the-board quality measures and two standardized PRO measures to evaluate quality of care for all patients and generated straightforward patient screening and EHR tools to gather patient data uniformly. They are now integrating those measures into the RISE registry to permit national benchmarking of lupus care (see table).2
“There are many things that we can do to improve the quality of care for people with SLE, because we know there are gaps in care, and we know there are a lot of health disparities in this disease,” Dr. Yazdany says. “What we have done is come up with five measures that provide a road map for what we want the future of SLE care to look like.”
Quality Measures

Dr. Jorge
The RISE registry is used to track a variety of quality measures for clinical care of patients with rheumatic diseases. “Clinicians can view the RISE dashboard to track how they are doing in terms of meeting those quality measures,” explains Dr. Jorge. “Previously, there were no lupus-specific quality measures, but it is important to improve quality care for patients with lupus.” Through this project, she and Dr. Bartels convened a 17-member panel of rheumatologists, nephrologists, patients and experts in quality measure development, with the goal of selecting three key measures.
Using a modified Delphi process, the panel began by reviewing relevant scientific literature in North America and Europe from 2000–2020 and synthesizing the evidence. They identified 57 possible quality constructs, which they narrowed to 15. “We created if-then statements for the 15 and summarized supporting evidence regarding the public health impact,” Dr. Bartels says. Through voting, they winnowed the list to three, and finally vetted them with patients to ensure they felt the measures would have clear patient benefit. The process and measures are detailed in a manuscript published in 2023.3
The three selected quality measures for SLE are:
- Hydroxychloroquine use for all patients without contraindications;
- Limits on the dose and duration of glucocorticoids not to exceed 7.5 mg/day of prednisone for longer than six months; and
- Regular kidney monitoring every six months to screen for and monitor lupus nephritis.
Regarding hydroxychloroquine, there are “good data showing that this drug reduces new organ involvement, cardiovascular disease and kidney disease,” Dr. Bartels says. “But when we talked to our patient advocates, who are very well informed and active in the lupus community, they actually had not had a conversation with their own doctors about how this one simple medicine can help them live longer. That highlighted to us that we need to make that message loud and clear.”
The second measure acknowledges that many adverse outcomes, including early stroke and early heart disease, are complications of glucocorticoids, as well as lupus itself. The measure’s recommendation to limit glucocorticoid use to no more than 7.5 mg daily by month six is consistent with EULAR and ACR guidelines, Dr. Bartels notes. “In fact, subsequent to our Arthritis Care & Research publication, EULAR is now recommending patients receive less than 5 mg. That may be a future benchmark for us, but for now our measure is staying at 7.5 mg, with the idea that patients and their doctors work together to switch to the steroid-sparing medicines that are now available.”
The third measure—regular kidney and urine screenings—is intended to detect SLE-caused lupus nephritis, which if left untreated can result in kidney failure. “Up to 50% of people with SLE can develop lupus nephritis, which may not have clear symptoms and could be missed unless specific screening laboratory tests are done,” Dr. Jorge says. “I hope this quality measure will help identify people with lupus nephritis early in the disease course, so they can be treated effectively.”
The work group is now planning discussions with the Centers for Medicare & Medicaid Services (CMS) to determine which measures to advance to payment programs. In addition, several RISE-enrolled rheumatology practices are collecting pilot data that the work group can compare with related EHR data from the RISE registry to make sure they match well. “If so, this will tell us that we can use EHR data from the RISE registry to accurately assess those quality measures,” Dr. Jorge says. “Our hope is to eventually apply these quality measures to the RISE registry, which will provide feedback to rheumatologists who are providing care to patients with lupus. The goal is to improve outcomes by improving quality care.”
Patient-Reported Outcomes
The second work group’s core team consisted of an expert work group, primarily physicians and researchers, along with “a wonderful and extremely brilliant patient, Wendy Rogers,” Dr. Yazdany says. The patient involvement didn’t end there. “We also had a full patient advisory group that participated in parallel with the expert work group, and the patient advisory group commented, provided feedback and voted every single step of the way, so the advisory group’s voice has profoundly influenced the measures that we ended up with.”
To determine which PROs to include, the expert work group pored through the foundational literature to identify outcome domains important to patients with SLE. With input from the patient advisory group, they selected the domains they felt were most valuable in providing patient care. After additional rounds of discussions, the work group identified depression and physical function as domains that should be part of the minimum standard of care for every patient. The work group detailed the selection process in an article published in January in Arthritis Care & Research.4
The expert work group and patient advisory group recommended:
- Assessment for depression at least once a year using the Patient Health Questionnaire or Patient Reported Outcomes Measurement Information System (PROMIS) depression scales;5,6 and
- Assessment of physical function at least once a year with the PROMIS physical function scales or the Multi-Dimensional Health Assessment Questionnaire (MDHAQ).7

Dr. Katz
Standardization of screening is important so that “everybody is using the same yardstick,” Dr. Katz says. Data collected in a consistent manner across EHRs and in the RISE registry can allow for rigorous research into not only the effectiveness of different treatments, but also possible disparities in treatments or outcomes, which can then enable building policies to address them.
The work group is now running a small pilot of the depression and physical function screenings, Dr. Katz says. “We have five test practices participating, and we’ll be having conversations soon to see how the screenings are working and whether the practices find the data of value. This is the information we need so we can make adjustments and, eventually, make the bigger effort to roll this out nationally.”
The pilot study will also explore whether rheumatology practices are comfortable conducting the screenings in routine care. For example, Dr. Yazdany says, rheumatologists often feel screening for depression is better relegated to the primary care setting. The patient advisory group, however, was adamant that rheumatologists are better equipped in that arena because they understand the struggles of lupus patients far better than do primary care doctors, who may only care for one lupus patient.
A further step will be to conduct a pilot study to delve into how rheumatologists may use the results of depression assessments. “Do they refer patients back to their family care doctor? Do they deal with a high score on a depression assessment themselves? Do they provide resources to the patients? This is not a trivial thing,” Dr. Yazdany remarks. “We need to figure out what to do with the information, and this is another area where our five pilot practices will help.”
The screenings are vital, Dr. Katz says. “Most of the clinical measures of lupus are really physician facing; these assessments give the patients the opportunity, in a standardized way, to express how they’re doing and bring [their] voice into regular lupus monitoring, [as well as] opens the door to support for depression or physical function, if needed. Beyond that, it also gives the patients tools to monitor themselves over time and, overall, gives them more agency in a clinical setting.”
Once the PRO work group has data from the pilot practices, it also hopes to begin building these measures into the RISE registry. “All of this work will be completed in the next two years, by the end of the grant,” Dr. Yazdany says. “It’s an ambitious project, but a really important one.”
Overall Goals
“It’s been a pleasure to work on this project,” Dr. Jorge says. “As we developed the EHR-based quality measures for lupus care, we have been very intentional at every step of the way about including perspectives from patients with lupus and from rheumatologists who utilize the RISE registry.”
The groups hope to eventually apply the quality and PRO measures to the RISE registry, where they can provide helpful feedback to rheumatologists who care for patients with lupus. “They will be able to see their own reported data, so they can look at the changes, make improvements and, perhaps, reach out to those patients who are struggling, so they can get them back into the office and either try something different or get them a referral. I think there will be some great opportunities there,” Dr. Bartels says. She believes the data will encourage rheumatologists to think creatively “so we can close care gaps and improve outcomes for patients.”
The overall goal for the project is to meet all five measures for all lupus patients by 2030, Dr. Yazdany says. “If people get these things—regular kidney and urine screenings for lupus nephritis; a hydroxychloroquine regimen, which we know is helpful in many ways; limitations on [glucocorticoids], which have numerous side effects; and annual assessments for depression and physical function—it will improve outcomes and hopefully reduce health disparities in this disease.”
The emphasis on lupus will continue beyond the end of the grant in 2025. “This project has helped to identify a pathway forward and has also been instrumental in the ACR obtaining additional funding from the Gordon and Betty Moore Foundation to examine the diagnostic pathway for lupus nephritis,” says Dr. Bartels. “I believe this project work is going to be really important for the future by bringing these measures to practice, and by encouraging discussions about what we can do to support improved care. I’m just excited to see this area move forward to help patients with lupus.”
Leslie Mertz, PhD, is a freelance science journalist based in northern Michigan.
References
- American College of Rheumatology. About the RISE Registry.
- Yazdany J, Jorge A, Barber C., et al. Healthy People with Lupus 2030: goals to improve the quality of care and health of all people with lupus in the United States. ACR Convergence 2023, San Diego, Calif.; abstract 1899.
- Bartels CM, Jorge A, Feldman CH, et al. Development of American College of Rheumatology quality measures for systemic lupus erythematosus: A modified Delphi process with Rheumatology Informatics System for Effectiveness (RISE) registry data review. Arthritis Care Res. 2023 Nov;75(11):2295–2305.
- Katz PP, Barber CEH, Duarte-García A, et al. Development of the American College of Rheumatology’s patient-reported outcome quality measures for systemic lupus erythematosus. Arthritis Care Res. 2024 Epub Jan 15. doi: 10.1002/acr.25301.
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001 Sep;16(9):606–613.
- PROMIS Health Organization. What is PROMIS?
- Agency for Healthcare Research & Quality. Multi-Dimensional Health Assessment Questionnaire (MDHAQ).