Monica Schroeder / Science Source
Stroke and transient ischemia are the most common cerebrovascular events in lupus patients, and a new study has found most of these occurrences can be attributed to lupus itself rather than other causes.
The study, published in the October 2018 issue of Arthritis Care & Research, looked at the frequency, association and outcomes of cerebrovascular events from a large, multi-ethnic cohort of patients with systemic lupus erythematosus (SLE).1 The study was conducted by the Systemic Lupus International Collaborating Clinics (SLICC) in 36 academic medical centers in 12 countries. The SLICC research network has been in existence for 27 years and has conducted a number of pivotal research initiatives in SLE, including recruitment to a large SLE disease inception cohort of more than 1,800 patients.
Led by John Hanly, MD, FRCPC, a rheumatologist at the Queen Elizabeth II Health Services Centre and a professor of Rheumatology at Dalhousie University Medical School, Halifax, Nova Scotia, Canada, the study sought to identify the frequency, characteristics and outcomes of cerebrovascular events, as well as clinical and autoantibody associations, in a multi-ethnic/racial inception cohort of patients with SLE. Dr. Hanly has been studying the impact of lupus on the nervous system for more than 30 years, and his research examines which problems are related to lupus and which are not. The answers will impact prognosis and treatment for lupus patients.
“We found cerebrovascular events, such as stroke and transient ischemia, are the fourth most common [type of] neuropsychiatric event in patients with SLE, with a prevalence of 4.5%,” Dr. Hanly says. “We also discovered that most cerebrovascular events, especially those that occur early in the disease course, can be directly attributed to lupus itself rather than to atherosclerosis.”
Cerebrovascular events that occur later in the disease course may be more frequently attributed to atherosclerosis, but Dr. Hanly says further follow-up is required to confirm this.
Dr. Hanly’s study looked at 1,826 patients with SLE (approximately 89% women, 49% Caucasian, with a mean age of 35 years). The large multi-ethnic/racial group was evaluated annually to assess clinical outcomes and mechanisms of cerebrovascular events in SLE.
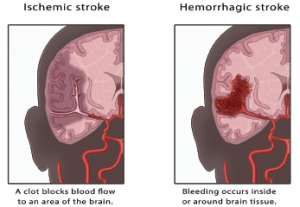
All of the participants were evaluated for common neuropsychiatric events, including five types of cerebrovascular events: stroke, transient ischemic attack (TIA), chronic multifocal ischemia, subarachnoid intracranial hemorrhage and sinus thrombosis.
“Of the 109 [cerebrovascular events] reported in a group of 1,826 SLE patients during a mean of 6.6 years of follow-up, 55% were stroke and 25.7% were transient ischemia,” Dr. Hanly says. “And 94% were considered SLE related.”
In contrast to good physician-reported outcomes, patients in the study reported a sustained reduction in health-related quality of life following a cerebrovascular event.



