Monica Schroeder / Science Source
Stroke and transient ischemia are the most common cerebrovascular events in lupus patients, and a new study has found most of these occurrences can be attributed to lupus itself rather than other causes.
The study, published in the October 2018 issue of Arthritis Care & Research, looked at the frequency, association and outcomes of cerebrovascular events from a large, multi-ethnic cohort of patients with systemic lupus erythematosus (SLE).1 The study was conducted by the Systemic Lupus International Collaborating Clinics (SLICC) in 36 academic medical centers in 12 countries. The SLICC research network has been in existence for 27 years and has conducted a number of pivotal research initiatives in SLE, including recruitment to a large SLE disease inception cohort of more than 1,800 patients.
Led by John Hanly, MD, FRCPC, a rheumatologist at the Queen Elizabeth II Health Services Centre and a professor of Rheumatology at Dalhousie University Medical School, Halifax, Nova Scotia, Canada, the study sought to identify the frequency, characteristics and outcomes of cerebrovascular events, as well as clinical and autoantibody associations, in a multi-ethnic/racial inception cohort of patients with SLE. Dr. Hanly has been studying the impact of lupus on the nervous system for more than 30 years, and his research examines which problems are related to lupus and which are not. The answers will impact prognosis and treatment for lupus patients.
“We found cerebrovascular events, such as stroke and transient ischemia, are the fourth most common [type of] neuropsychiatric event in patients with SLE, with a prevalence of 4.5%,” Dr. Hanly says. “We also discovered that most cerebrovascular events, especially those that occur early in the disease course, can be directly attributed to lupus itself rather than to atherosclerosis.”
Cerebrovascular events that occur later in the disease course may be more frequently attributed to atherosclerosis, but Dr. Hanly says further follow-up is required to confirm this.
Dr. Hanly’s study looked at 1,826 patients with SLE (approximately 89% women, 49% Caucasian, with a mean age of 35 years). The large multi-ethnic/racial group was evaluated annually to assess clinical outcomes and mechanisms of cerebrovascular events in SLE.
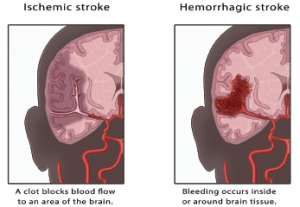
All of the participants were evaluated for common neuropsychiatric events, including five types of cerebrovascular events: stroke, transient ischemic attack (TIA), chronic multifocal ischemia, subarachnoid intracranial hemorrhage and sinus thrombosis.
“Of the 109 [cerebrovascular events] reported in a group of 1,826 SLE patients during a mean of 6.6 years of follow-up, 55% were stroke and 25.7% were transient ischemia,” Dr. Hanly says. “And 94% were considered SLE related.”
In contrast to good physician-reported outcomes, patients in the study reported a sustained reduction in health-related quality of life following a cerebrovascular event.
Improving Prognosis & Treatment
Previous studies have found patients with SLE are at a higher risk of stroke than the general population, regardless of the type of stroke, and that the relative risk is greater in younger patients.2 These studies show most cases of stroke occurred in the first five years of the disease, particularly during the first year, emphasizing the importance of screening for modifiable risk factors to guide prevention strategies at the time of diagnosis of SLE.
Increasing awareness of the risk of stroke in patients with SLE may help prevent strokes & minimize disability, if the risk is identified early.
Dr. Hanly notes that increasing awareness of the risk of stroke in patients with SLE may help prevent strokes and minimize disability, if the risk is identified early. He recommends screening all patients diagnosed with SLE for traditional cerebrovascular events at the time of diagnosis and annually thereafter.
Dr. Hanly also notes stroke rates are higher in SLE patients of African ancestry. Another recent study, published in Seminars in Arthritis & Rheumatism, showed that certain races were disproportionately affected by cerebrovascular events.3 The study found that black SLE patients in the U.S. are at a 34% higher risk of stroke than white patients, while Hispanics had a 25% greater risk.
The study, conducted by researchers in Boston and New York, identified 65,788 SLE patients between the ages of 18 and 65 and found that after conducting a mean follow-up of 3.7 years, 1,441 first-stroke events were recorded (1,208 ischemic and 233 hemorrhagic). In conducting their analysis, researchers took into account such risk factors as hypertension, heart failure and cardiovascular disease, as well as medication use and sociodemographic factors.
Although the mortality rate for SLE has improved over the past three decades, Dr. Hanly says the mortality rate for lupus patients remains high relative to non-lupus populations.
According to the Centers for Disease Control and Prevention, SLE is the 10th leading cause of death in women ages 15–24 and the fifth leading cause of death for black and Latina women in that cohort.4
“We have one approved biologic currently being used to treat SLE, [and] a number of investigational drugs [are] being tested in clinical trials,” Dr. Hanly says.
As for current treatment guidelines, Dr. Hanly notes that, due to the potential side effects, there isn’t enough evidence to recommend putting all SLE patients at high risk on anticoagulants.
“There are other, safer lifestyle measures that can reduce the risk of stroke, including maintaining a healthy body weight, reducing hypertension, quitting smoking, engaging in regular daily exercise and keeping high cholesterol and diabetes in check,” Dr. Hanly says. “Future studies [may] provide new insights and information that can be used in developing individualized treatment plans.”
Linda Childers is a health writer located in the San Francisco Bay Area.
References
- Hanly JG, Li Q, Su L, et al. Cerebrovascular events in systemic lupus erythematosus: Results from an international inception cohort study. Arthritis Care Res (Hoboken). 2018 Oct;70(10):1478–1487.
- Barbhaiya M, Feldman CH, Guan H, et al. Racial/ethnic variation in stroke rates and risks among patients with systemic lupus erythematosus. Semin Arthritis Rheum. 2019 Apr;48(5):840–846.
- Krishnan E. Stroke subtypes among young patients with systemic lupus erythematosus. Am J Med. 2005 Dec;118(12):1415.
- Yen EY, Singh RR. Brief report: Lupus an unrecognized leading cause of death in young females: A population-based study using nationwide death certificates, 2000–2015. Arthritis Rheum. 2018 Aug;70(8):1251–1255.



