Sites at which regulatory factors control osteoclast differentiation and activity include bone-lining cells affected by PTH, PTH-related peptide (PTHrP—the humoral factor associated with hypercalcemia of malignancy), 1,25 OH2 Vit D3, prostaglandin E2, and cytokines IL-1, TNFα, IL-11 and IL-17. Factors including M-CSF, RANKL, IL-1, TNFα, IL-6, IL-11 and IL-15 act on osteoclast precursors to induce differentiation into osteoclasts.14
Several factors act on osteoclasts directly to enhance resorption, including IL-1, TNFα and RANKL. As demonstrated in multiple studies, RANKL is important in focal bone loss in RA. RANKL mRNA and protein are expressed in synovial tissue in patients. Expression is localized in synovial fibroblasts and T cells, which may induce osteoclastogenesis in vitro. Of note, however, is that treatment of cell cultures with OPG did not completely block osteoclastogenesis, as might be expected, which suggests that other proteins or factors from synovial cells may also have osteoclast-inducing potential.14
Cartilage destruction in RA can occur through direct release of products in pannus that degrade the matrix, specifically MMP and cathepsins. Indirect mechanism involves release of pannus-derived cytokines, which induce chondrocytes to release factors that degrade the matrix, including nitric oxide (NO), IL-1 and TNFα.14
There is compelling data to suggest that TNFα antagonists have an effect on NO production in human cartilage. Osteoarthritic cartilage (OA) produces NO, which is stimulated by proinflammatory cytokines TNFα, IL-1β, IL-17 and bacterial lipopolysaccharide.16
Both infliximab and etanercept, TNFα antagonists, inhibited TNFα-induced NO production in a dose-dependent mechanism with no evidence of any impact on IL-1β, IL-17 and LPS stimulated synthesis. Data from the study suggests that endogenous-cartilage-derived TNFα antagonists modulate NO production in the cartilage of OA patients. TNFα and soluble TNFα receptor (sTNFRI and sTNFRII), both made by human OA cartilage, when subjected to a neutralizing antibody, enhanced NO production against sTNFRI, but not against sTNFRII. This suggests that TNFα is not an autocoid (hormone-like substance) mediator in these functions.16
Conclusion
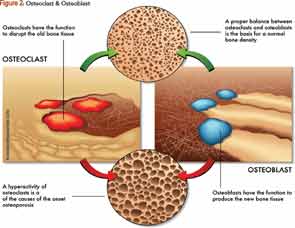
Understanding pathways of bone remodeling, including bone resorption and bone formation, is the key to future research and development of newer therapies for the prevention and treatment of osteoporosis. With the aging population in our country, the impact of menopause and the potential effects of certain medications, we are at risk for fragile bones and fracture. As rheumatologists, we need to continue to encourage nonmedical interventions for our younger population that can enhance their optimal peak bone mass. Additionally, there should be a major focus on nutrition, exercise and lifestyle modifications, all of which contribute to better bone health.