Earlier this summer, the National Center for Health Statistics’ Coordination and Maintenance Committee (CMC) for the International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) approved a new code for non-radiographic axial spondyloarthritis (nr-axSpA), effective Oct. 1. The ICD-10-CM is a morbidity classification published by the U.S. for classifying diagnoses and reason for visits in all healthcare settings. It’s based on the ICD-10, the statistical classification of disease published by the World Health Organization.
The new diagnostic code should make it easier for rheumatologists to bill for treatment of nr-axSpA, a form of arthritis that causes inflammation in the spine and sacroiliac joints and may lead to severe, chronic pain and impairment of spinal mobility. The code can also be used to track and mine its incidence in electronic health records, enabling new research strategies for improving treatment.
The ACR’s Committee on Rheumatologic Care supported the proposal through the approval process alongside global biopharmaceutical company UCB, Brussels, and patient advocacy groups. UCB manufactures the biologic treatment certolizumab pegol (Cimzia), a tumor necrosis factor blocker approved by the U.S. Food & Drug Administration on March 29, 2019, as the first treatment for nr-axSpA.1 UCB has been pursuing the new ICD-10-CM code for two years, says Jeffrey Stark, MD, an Atlanta-based rheumatologist and UCB’s head of medical immunology. Two other drugs have subsequently been approved for the condition, secukinumab (Cosentyx, Novartis) and ixekizumab (Taltz, Lilly). Clinicaltrials.gov currently lists 20 studies of treatments in the pipeline for nr-axSpA.2
The existence of three approved drugs for this condition highlights the divide between ICD-10 and current clinical practice, Dr. Stark says. European countries are already moving toward implementing the 11th revision of ICD, which includes recognition of nr-axSpA.
“We submitted our application to the CMC several times over the past two years, but we weren’t always included on the agenda for [its] twice-yearly meetings,” Dr. Stark explains.
After being asked to resubmit the application with more justification, UCB approached the ACR, says Colin Edgerton, MD, a rheumatologist in North Charleston, S.C., and chair of the ACR’s Committee on Rheumatologic Care (CORC). CORC supported the proposal along with patient advocacy groups. Drs. Edgerton and Stark both describe the process as a great example of aligned groups working together to support patients’ best interests.
The latest submission, made last September with a support letter from the ACR and alignment with the patient community, was approved in June and announced through the release of CMC’s larger document of ICD-10 updates.3 The threshold for making a change to ICD-10 is high, Dr. Stark says. “They don’t take modifications lightly, and they really require a demonstrable clinical need, articulated by the provider community.” And that’s where the ACR came in.
Ending a Bureaucratic Nightmare
“We are happy to see this new code approved. The subject is of great interest for a disease that was recognized fairly recently,” says Dr. Edgerton. “Now that we have a way to document it, we expect to see improvements in care and in generating real-world evidence about it while making it easier for clinicians to speak the same language about it.”
The new code is also a step toward better defining and understanding the spectrum of spondyloarthritic diseases, which previously was defined largely by X-rays. “Now we’re getting more sophisticated at recognizing these subgroups, which have similar inflammatory arthritis of the spine. But much remains to be understood,” Dr. Edgerton says.
Dr. Stark estimates that 1.7 million people in the U.S. are living with nr-axSpA. The condition presents no X-ray evidence of structural damage to the sacroiliac joints, even though patients may have high symptom burden. A roughly equal number of people have the related condition, ankylosing spondylitis (AS), which is diagnosed with definitive X-ray evidence of structural change to the sacroiliac joints. An unknown number of patients will progress from a non-radiographic diagnosis to AS, and that can take years.
What sometimes happens, Dr. Stark adds, is that it can take five to eight years for a patient with back pain to reach a rheumatologist’s office and be given a diagnosis of nr-axSpA, which is often mistaken for other conditions. “These people can have an incredible journey to get to a diagnosis.” For the patient to finally reach the rheumatologist’s office and then be told that their condition cannot be documented because of coding limitations has been frustrating.
If the doctor prescribes treatment for a condition for which there is no code, the insurer’s verification process may not recognize it, thus triggering a claim denial, Dr. Edgerton says. The denied claim then has to go through an appeal process. “It’s a bureaucratic nightmare, all because there’s no code for this condition.”
The new code should help reduce the chance that an appropriate treatment prescribed for nr-axSpA would be denied by a payer. Now that the new code has a projected live date, EMR vendors will be updating their databases to include it. ACR members who have questions should reach out to the College for correct coding guidelines and ongoing updates, says Antanya Chung, ACR’s director of practice management. “As we get the code going, we’ll have more to add.” Ms. Chung can be reached at [email protected].
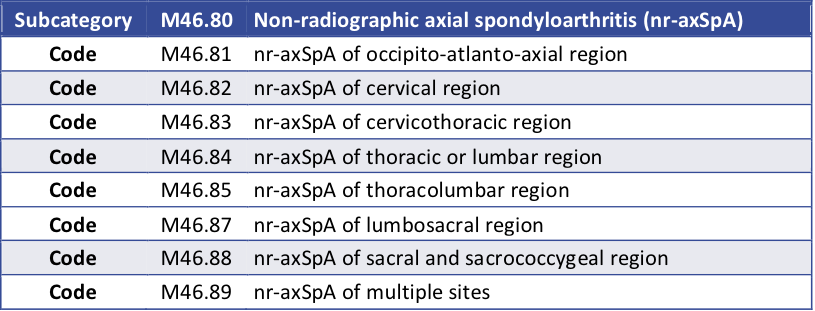
Table 1: According to the National Center for Health Statistics’ ICD-10-CM Coordination and Maintenance Committee, the proposed ICD-10-CM codes for non-radiographic axial spondyloarthritis are:
References
- U.S. Food & Drug Administration. FDA approves treatment for patients with a type of inflammatory arthritis.
- Clinicaltrials.gov. U.S. National Library of Medicine.
- ICD-10 Coordination & Maintenance Committee, U.S. National Center for Health Statistics. FY 2021 ICD-10-CM Official Coding and Reporting Guidelines. July 2020.
Larry Beresford is a medical journalist in Oakland, Calif.


