
Thumb carpometacarpal (CMC) joint osteoarthritis (OA) is the second most common form of hand OA, affecting between 20% and 30% of the general population.1,2 Thumb CMC joint OA is more prevalent in females than males, increases with age, and has been associated with hand pain and loss of functional hand use.3 While CMC arthroplasty and fusion are options for patients, they may not be optimal. This article describes how OA can affect hand anatomy and kinematics, and discusses conservative interventions including splinting, exercise techniques, and physical agent modalities.
Anatomy of the Thumb CMC Joint
Bony articulation: The trapezium bone of the wrist and the first metacarpal of the thumb comprise the thumb CMC joint. The biconcave/biconvex nature of the articulating surfaces of the thumb CMC joint is unique: the trapezium is shaped like a saddle with both a concave surface and a convex surface, and the first metacarpal has corresponding convex and concave surfaces.4 The unique shape of the articulating surfaces allows for movement in flexion/extension, abduction/adduction, and the combined planar movement of opposition.
Ligaments: The ligaments of the thumb CMC joint are the anterior oblique ligament, posterior oblique ligament, radial collateral ligament, ulnar collateral ligament and intermetacarpal ligament. As a group, the ligaments guide the movement of the first metacarpal on the trapezium and serve to check excessive movement and unwanted joint play, which provide joint stability. All of these ligaments restrain the movement of opposition. The anterior oblique and ulnar collateral ligaments also check extension while the radial collateral ligament checks adduction. The anterior oblique ligament, which connects the anterior tubercle on the trapezium to the anterior surface of the metacarpal, is also termed the “beak” ligament.
Joint kinematics: The thumb joint moves in multiple planes. With the forearm in neutral position, the “hitchhiking” upward movement of the thumb is extension, and movement downward in the plane of the palm is flexion. A 90-degree movement of the thumb away from, and return to, the index finger is abduction and adduction, respectively. Opposition is defined as axial rotation of the thumb resulting in the pad of the thumb facing the pads of the digits. Thumb opposition to the small finger is a complex multiplanar movement. It begins with abduction. The metacarpal then rotates inward around the longitudinal axis to face the pads of the digits.
The convex/concave rules of joint motion apply to the movements of abduction/adduction and flexion/extension. During abduction/adduction, the convex base of the thumb metacarpal glides laterally on the concave portion of the trapezium. During flexion/extension the concave portion of the thumb metacarpal both glides and rolls toward the direction of the movement on the convex portion of the trapezium.
The motions of this unique joint can be appreciated through palpation. To accurately locate the thumb CMC joint and feel the kinematics of abduction, palpate the lateral surface of the head of the thumb metacarpal at the metacarpophalangeal (MP) joint. Slide the palpating digit down to the flared base of the thumb metacarpal. Adduct the thumb while maintaining this palpating position. As described above, the base of the metacarpal will glide laterally and become prominent under the palpating digit. The trapezium is just proximal to the base of the metacarpal and remains stationary during the movement. To palpate flexion of the thumb across the palm, move from the lateral position to the base of the thumb metacarpal on the dorsal aspect. The metacarpal base can be palpated as it rolls and glides towards flexion.
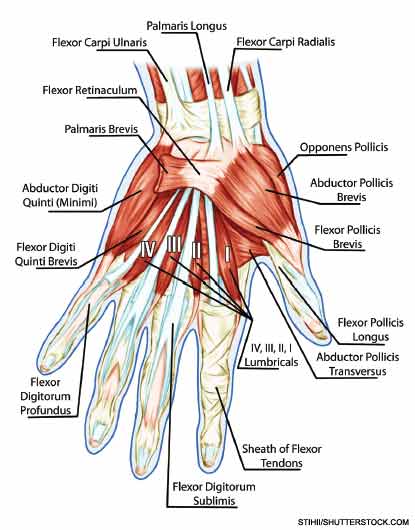
Muscle activity: Muscles that cross the thumb CMC joint include the flexor pollicis longus and brevis, adductor pollicis, abductor pollicis longus and brevis, extensor pollicis longus and brevis, and opponens pollicis (see Figure 1). The median nerve-innervated thenar muscle group is composed of the opponens pollicis, abductor pollicis brevis, and half of the flexor pollicis brevis. The primary purpose of the abductor pollicis longus and brevis, and the extensor pollicis longus and brevis, is to position the thumb. An example would be opening the hand in preparation to grasp a cylindrical glass. These muscles do not typically produce significant forces. The opponens pollicis also positions the thumb, rotating the pad of the thumb to face the pads of the fingers in preparation for pinching activities. The muscles that supply significant force during grasp or pinch activities are the flexor pollicis longus and brevis, and adductor pollicis.
Pathomechanics of the Thumb CMC Joint
Ligamentous laxity and joint impingement: The movements at the thumb CMC joint explain the characteristic problems seen with thumb CMC joint OA. Laxity in the anterior oblique or “beak” ligament can predispose the thumb CMC joint to excessive pressure on the volar portion of the trapezium, particularly during lateral pinch activities such as holding a key.5 With beak ligament laxity, resisted pinching can lever the base of the metacarpal dorsally, resulting in volar compression and posterior translation of the base of the metacarpal. The dorsal/lateral subluxation of the metacarpal base produces the “shoulder sign,” a lateral prominence of the CMC joint, which has been associated with CMC OA (see Figure 2).

Research suggests that compression caused by grip-and-pinch activities occurs over a relatively small surface area between the metacarpal and the trapezium and can lead to uneven wear patterns. Momose and colleagues examined the area of contact on the trapezium by the first metacarpal during various thumb movements.6 Their findings generally support what would be predicted by the convex/concave rules of joint motion. During opposition, the contact area on the trapezium was in the radial, volar, and ulnar segments. During abduction the contact area was in the dorsal segment.
Another notable finding of this study was the relatively small area of contact measured at the end ranges of movement. For opposition, the contact area measured approximately 50% of the articulating surfaces. For abduction, the contact area was approximately 25%. Microscopic analysis of cadaveric hands with thumb CMC joint OA identified that the location of greatest cartilage degeneration within the thumb CMC joint was in the dorsal radial region of the trapezium.7 One goal of therapy is to maintain maximum contact between articulating surfaces during joint motion to reduce compression within the joint. This can prevent uneven wear patterns in the thumb CMC joint and lessen the potential for cartilage deterioration. Knowledge of patients’ wear patterns can help physicians and therapists select management strategies for patients.
Muscle considerations: Forceful thumb use is required to hold objects between the thumb and fingers. As muscle force increases, so does the compression force between the trapezium and metacarpal. Pinching forces occur at the interface between the thumb and the fingertips in the case of a tip-to-tip or pad-to-pad pinch, and between the pad of the thumb and the lateral border of the index finger in the case of a lateral pinch. In either case, these forces occur approximately three to four inches from the axis of rotation at the thumb CMC joint. As described earlier, the muscles that generate forceful pinch cross the thumb CMC joint and act upon it. Pinching, an isometric activity, results in compression at the thumb CMC joint. Cooney calculated that the compression forces at the thumb CMC joint were approximately 12 times the pinching forces that occur at the thumb pad.8
Muscle imbalances between the finger muscles and thumb muscles also increase stress on the CMC joint. If the thumb muscles are weak in comparison to the finger muscles, the CMC joint will shift slightly into a position that increases point pressure within the joint during pinch. For example, during pad pinch the force of the finger muscles will produce thumb extension and abduction if unopposed by the thumb muscles. If the thumb muscles are incapable of resisting the force of the finger muscles, slight abduction and/or extension may occur, resulting in increased compression in the dorsal radial aspect of the trapezium. Beak ligament laxity will cause dorsal subluxation of the metacarpal, leading to volar surface compression on the trapezium. Opposition limited by weakness of the opponens, adductor tightness, or soft-tissue limitations of the web space will further exacerbate the problem. Figure 3a shows a pinching activity with good thumb and finger muscle balance while Figure 3b shows the same activity with limitations in thumb opposition. The stronger finger muscles, in addition to unstable ulnar collateral ligaments of the interphalangeal (IP) and MP joints, force the thumb into noticeable abduction at the IP and MP joints and more subtle abduction at the CMC joint. These positions result in point compression in the dorsal radial aspect of the trapezium.


Conservative Treatments for Thumb CMC Joint OA
Thumb CMC joint OA affects the stability and kinematics of the joint. The thumb acts as a stable post during hand tasks, particularly pinch tasks. Pinch tasks can place tremendous amounts of force on the CMC joint, which can exacerbate any underlying loss of stability. These changes may lead to pain and hand disuse, further reducing thumb muscle strength. Reduced muscle strength, and the resulting imbalances, can further exacerbate thumb CMC joint OA. Conservative treatments for thumb CMC joint OA focus on reducing the forces acting on the joint by providing supportive splints, improving muscle strength, and teaching patients joint-protection techniques.
Prior to the introduction of any conservative technique, therapists take a detailed history of the patients’ onset of pain and symptoms. They identify how patients use their hands for daily tasks and identify unique functional requirements of each hand. These evaluations may include: dominant versus non-dominant hand use; specific hand-use requirements for vocational and avocational activities; and specific tasks that aggravate patients’ symptoms such as writing, tool use, and cane or walker use. Patients are encouraged to gain insights as to how, when, where, and why their symptoms are aggravated. This information can help therapists select appropriate splint designs, exercise regimens, modality use, and educational requirements for patients.
Splinting: Splints are a common and effective treatment that reduce pain and increase function in patients with thumb CMC joint OA. The purpose of splints for these patients is to support structures that have lost their integrity. As noted earlier, ligamental attrition is common in thumb CMC joint OA. This lack of ligamental support allows the metacarpal to translate over the trapezium during pinching activities, causing a grinding in the joint, and eventually pain with pinch-and-grasp activities. Functionally, anything that is done with the hands includes grip-and-pinch activities, so support of the joint is essential. A splint designed to support the thumb CMC joint during pinching prevents thumb translation and allows for pain-free, functional hand use.9 A recent systematic review supports the use of splinting, finding that patients who used splints had reduced pain, as well as reduced translation of their CMC joint during pinching activities.10
The hand-based thumb spica splint is the most common type of splint provided to patients with thumb CMC joint OA (see Figure 4). The spica splint is designed to prevent CMC translation or movement beyond the normal joint glide, essentially replacing unstable ligaments. Therapists fabricate hand-based spica splints to incorporate the functional anatomy and posture of the thumb and hand during use. The splint stabilizes the base of the thumb in opposition and leaves the thumb tip, fingers, and wrist unrestricted. This allows for full functional use while protecting the thumb CMC joint.

To fabricate a successful thumb spica splint, therapists collaborate with patients to construct splints that facilitate functional requirements. For example, patients who handle large cylindrical objects, such as tool handles, have different grip-and-pinch requirements than those who handle a needle. Splint fabrication may require multiple attempts to identify patients’ thumb-and-hand functional requirements and construct one or more splints to facilitate functional activity.
Exercise: Weakness of thumb musculature leads to an imbalance of forces between the thumb and fingers. This imbalance can cause abnormal wear on the trapezium and metacarpal joints. Exercises to strengthen the thumb muscles can reduce this imbalance and also increase muscle-related stability around the thumb CMC joint. Studies that have examined the role of exercise in treating thumb CMC joint OA report improvements in strength, pain, and hand function.9
While not specific to the thumb CMC joint, Stamm et al reported a significant improvement in grip strength and improved global hand function scores in patients with hand OA given joint protection education and hand exercises.11 The exercises given to the experimental group consisted of tendon gliding and active thumb opposition. Pelligrini et al recommends thenar strengthening to promote a stable joint position during pinching activities.5 Boustedt et al found that adding splinting and exercises to joint-protection education resulted in improved pain control and daily function.12

As described above, resistive activity/exercise of the muscles that cross the CMC joint of the thumb results in joint compression that may contribute to cartilage deterioration and pain. Therefore, any strengthening exercise program for thumb CMC joint OA should be completed under the supervision of a therapist and structured to be pain-free and prevent excessive joint compression. During periods of acute inflammation, patients should perform pain-free active range of motion for all thumb movements to maintain tendon gliding and joint mobility.
Therapists evaluating patients with thumb CMC joint OA can determine if joint instability or weakness contributes to uneven joint compression and pain during specific functional tasks and develop patient-specific exercises. For example, resistive lateral pinch activities such as squeezing out toothpaste may cause pain and dorsal subluxation of the base of the metacarpal. The therapist provides the patient with pain-free, isometric thumb flexion and adduction exercises to improve this functional task. Patients are encouraged to determine which joint positions improve stability and decrease pain during functional tasks. Isometric strengthening of the muscles that maintain optimum positioning can then be provided.
Therapists also assess web space extensibility. Patients with limited web space extensibility will have a decreased ability to position their thumbs in true opposition, resulting in less stable joint positions and increased lateral forces applied to the thumb. Gentle stretching of the web space can be included in the exercise program if decreased web space extensibility is present.
Thermal physical agent modalities (PAMS): Although there is only weak-to-moderate evidence to support the use of thermal PAMS, some patients may experience pain relief with the application of ice or heat.9 Therapist preference and patient response guide modality use. Some patients with high levels of pain may feel relief with cryotherapy, yet others prefer not to have cold on their hands. Paraffin baths and heat wraps can also provide relief.13
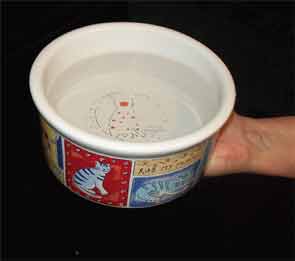
Joint protection: In joint-protection programs, patients are trained to be aware of how various activities affect their joints and modify how they perform activities to reduce joint stress. There are several principles of joint protection: using larger, more stable joints during activities; providing appropriate rest or break periods; decreasing muscle force; and using adaptive equipment if appropriate. For example, a patient with thumb CMC joint OA could be taught to avoid tasks that require significant thumb force such as lateral-pinch activities (see Figure 5a), and trained to perform the task with larger joints (see Figure 5b). Patients can be provided with adaptive equipment, such as a built-up pencil grip to assist with writing or a wall-mounted jar opener (see Figure 6).

As with the splinting and exercise programs, therapists can determine joint-protection strategies based on patients’ activity profiles. The benefits of joint-protection programs have been extensively studied for patients with rheumatoid arthritis, but these principles have been found to be appropriate for people with OA as well.9,13 In a prospective study, Berggren et al examined the benefits of joint protection and splinting for thumb OA patients awaiting joint replacement surgery.14 Following a seven-month period, 70% of the patients no longer felt surgery was needed.
Thumb CMC joint OA can cause pain and disability. Conservative treatments provided by therapists who have expertise in hand-function issues, can reduce pain and improve function. Splints provide support and pain relief, allowing patients to use their hands for necessary occupations such as work and hobbies. Strengthening and stretching exercises reduce compressive forces by improving muscle balance and overall hand motion. Thermal physical agent modalities can provide pain relief. Joint-protection techniques can help patients manage their symptoms and provide them with knowledge on how to reduce stress on their joints. Physicians should consider referring patients for hand therapy as part of an overall strategy to reduce the impact of thumb CMC joint OA, and thus improve their quality of life.
Dr. Gustafson is an occupational therapist and Dr. Baker is an associate professor, both at the University of Pittsburgh in Pennsylvania. Dr. Jacobs is a senior occupational therapist at the University of Pittsburgh Medical Center’s Centers for Rehab Services.
References
- Wilder F, Barrett J, Farina E. Joint-specific prevalence of osteoarthritis of the hand. Osteoarthritis Cartilage. 2006;14:953-957.
- Haugen I, Englund M, Aliabadi P, et al. Prevalence, incidence and progression of hand osteoarthritis in the general population: The Framingham Osteoarthritis Study. Ann Rheum Dis. 2011;70:1581-1586.
- Marshall M, van der Windt D, Nicholls E, Myers H, Hay E, Dziedzic K. Radiographic hand osteoarthritis: Patterns and associations with hand pain and function in a community-dwelling sample. Osteoarthritis Cartilage. 2009;17:1440-1447.
- Neumann D, Bielefeld T. The carpometacarpal joint of the thumb: Stability, deformity, and therapeutic intervention. J Orthop Sports Phys Ther. 2003;33:386-399.
- Pellegrini VD. Pathomechanics of the thumb trapezioetacarpal joint. Hand Clin. 2001;17:175-184.
- Momose T, Nakatsuchi Y, Saitoh S. Contact area of the trapeziometacarpal joint. J Hand Surg Am. 1999;24:491-495.
- Kovler M, Lundon K, McKee N, Agur A. The human first carpometacarpal joint: Osteoarthritic degeneration and 3-dimensional modeling. J Hand Ther. 2004;17:393-400.
- Cooney W, Chao E. Biomechanical analysis of static forces in the thumb during hand function. J Bone Joint Surg Am. 1977;59:27-36.
- Beaseley J. Osteoarthritis and rheumatiod arthritis: Conservative therapeutic management. J Hand Ther. 2012;25:163-172.
- Egan M, Brousseau L. Splinting for osteoarthritis of the carpometacarpal joint: A review of the evidence. Am J Occup Ther. 2007;61:70-78.
- Stamm TA, Machold KP, Smolen JS, et al. Joint protection and home hand exercises improve hand function in patients with hand osteoarthritis: A randomized controlled trial. Arthritis Rheum. 2002;47:44-49.
- Boustetd C, Nordenskiöld U, Lundgren Nilsson AL. Effects of a hand-joint protection programme with an addition of splinting and exercise: One year follow-up. Clin Rheumatol. 2009;28:793-799.
- Valdes K, Marik T. A systematic review of conservative interventions for osteoarthritis of the hand. J Hand Ther. 2010;23:334-351.
- Berggren M, Joost-Davidsson A, Lindstrand J, Nylander G, Povlsen B. Reduction in the need for operation after conservative treatment of osteoarthritis of the first carpometacarpal joint: A seven year prospective study. Scand J Plast Reconstr Surg Hand Surg. 2001;35:415-417.


