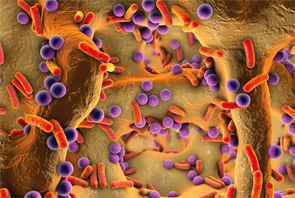
The discovery of the pivotal role of the human microbiome has challenged some of the long-held anachronistic views that considered all infectious agents to be evildoers.
Kateryna Kon/shutterstock.com
Which came first? The infectious microorganism or a host’s immune resistance against it?
Through the millennia, a raging battle has pitted the hordes of infectious agents surrounding us against, arguably, the most complex biologic structure ever created, the finely tuned human immune system. The stakes are high for both sides. For the infectious agent, an inability to penetrate the host defenses may lead to its imminent demise and an untimely death. For the host, letting its guard down can lead to some dire consequences including infection, illness or, if molecular mimicry holds true, the development of autoimmunity.
Yet life on our planet as we know it would cease without the presence of these pesky bugs. In fact, the discovery of the pivotal role of the human microbiome has challenged some of the long-held anachronistic views that considered all infectious agents to be evildoers. It may be hard to conceptualize that lurking within each and every one of us resides a population of well over 100 trillion bacteria, or 10-fold the number of cells in our bodies, that is estimated to weigh 5 lbs.1 These massive colonies of bacteria and their infinite generations of progeny have taken up lifelong residence within our gut, oral cavities, skin, lungs, eyes and elsewhere. Till death do us part.
What are they doing within? Some, if not most of these organisms bear no malice and contribute to our host defenses in most meaningful ways. For example, we are discovering their pivotal role in the pathogenesis of cancer, rheumatoid arthritis, inflammatory bowel disease and a host of other autoimmune diseases.2
In a similar vein, the human virome, the virtual home for all viral vectors lurking within, exerts its own profound influence on our lives in times of health and disease. Given the nanoscale size of viruses and their infectious snippets of DNA and RNA, it should come as no surprise to learn that the number of free virions just residing at body barrier sites, such as the gut, oropharynx and skin, may range as high as 109 particles per gram. Step aside, microbiome: It has been estimated that the human body may contain an eye-popping 1015 bacteriophages that regulate the structure and function of bacterial communities through their lytic and lysogenic cycles.3 Don’t forget to pass the hand sanitizer.
Protecting us from the hazards of an infectious onslaught are our two formidable pillars of resistance, the innate and adaptive immune systems—complex networks both, whose continuous surveillance of our bodies’ inner workings would fill a National Security Agency analyst with envy. We can only look with wonder at the agility and elaborate plasticity of the human immune response.
But even this wonderful system can be prone to an occasional error, leading to the development of an infectious or an autoimmune disease. Sometimes, it may be due to a hardware issue, as in cases of immune deficiency where key components, such as serum immunoglobulins, may be lacking, or a selective complement component deficiency may predispose the bearer to lupus. In other situations, there may be a software glitch resulting in a misinterpretation of immune and infectious signals. One might consider the development of chronic fatigue following the supposedly successful treatment of B. Burgdorferi infection to be such an example. And in other cases, our immune defenses may have completely misunderstood the sequence of events, misinterpreting an infectious disease for an autoimmune disorder.
Mistaken Identity
A prime example of this sort of misunderstanding is the disease formerly known as essential mixed cryoglobulinemia (EMC). Aside from its chill-inspiring name that over the years has confused many well-intentioned medical house staff and students into believing that a patient’s freshly drawn blood sample needed to be cryopreserved immediately rather than spun and separated first, there was a long-held belief that this condition arose from some form of immune perturbation. Hence the appellation, essential, an oft-used medical term employed when we are clueless about the cause of a disease.
It had long been understood that cryoglobulin deposition spelled trouble because the inflammation caused by the plugging of vascular lumina often led to tissue ischemia downstream. Affected individuals developed an illness with overlapping features of lupus, vasculitis and rheumatoid arthritis (RA). Coupled with the observation that cryoglobulins often demonstrated the binding capabilities of rheumatoid factors (RFs), it was assumed that EMC was, at its core, an autoimmune disorder.
The innovative investigations of the late Ed Franklin, MD, formerly of New York University in New York City, along with his colleague, the late Henry Kunkel, MD, formerly of the Rockefeller University in New York City, established our core understanding of EMC. Their seminal research led to the characterization of EMC being associated with polyclonal IgG targeting RF-containing cryoglobulins (type II cryoglobulinemia).4 Although they suspected that a viral agent, such as hepatitis B virus, might be the driver of all this RF activity, there was scant evidence to support this view.
Their hypothesis was finally proved about two decades later, but with an added twist, when it was discovered that there was indeed a breach of immune defenses. Hepatitis C virus (HCV) was discovered to be concentrated 1,000-fold in the cryoglobulin protein of affected individuals.5 Tearing a page out of a spy thriller, it turned out that a particular cryoglobulin idiotype could bind to very low-density lipid (VLDL)–like particles that masked HCV, allowing it to avoid detection when entering the liver cell attached to its LDL receptor.5
Nowadays, we consider EMC in a different light, as upward of 90% of patients are positive for HCV. More critical than renaming EMC as HCV-associated type II cryoglobulinemia has been the subsequent transformation of our treatment of this disease from requiring high doses of corticosteroids along with the frequent addition of cytotoxic drugs to a multisystem infectious illness requiring antiviral therapy targeting HCV.
Might there be other similar situations where we are mistakenly treating viral infections as autoimmune conditions? Lately, the neurology literature has been replete with clinical observations suggesting a link between the development of strokes following exposure to varicella zoster virus (VZV).6 This virus has been implicated in some cases of aortitis, and its role has also been questioned in the pathogenesis of giant cell arteritis.7 Beneath the painful, itchy dermatomes, might VZV be wreaking even more havoc deep inside by promoting damaging inflammatory responses within our vasculature?
Given the nanoscale size of viruses & their infectious snippets of DNA & RNA, it should come as no surprise to learn that the number of free virions just residing at body barrier sites, such as the gut, oropharynx and skin, may range as high as 109 particles per gram. Step aside, microbiome: It has been estimated that the human body may contain an eye-popping 1015 bacteriophages that regulate the structure & function of bacterial communities through their lytic & lysogenic cycles.
Blurred Lines
Indeed, the lines separating infection and immunity can get quite blurred. Consider the case of Kawasaki’s disease (KD), an uncommon pediatric disorder that was first recognized in Japan in the 1960s by a Japanese pediatrician, Tomisaku Kawasaki, MD. He and others described young children, often boys, presenting with fever, cutaneous lesions and swollen appendages.8 Beneath this outward visage of an infectious illness, though one without a defined cause, lay a rare but potentially lethal complication, the formation of coronary aneurysms in the young child’s heart.
Over the ensuing decades, the Japanese birthrate continued to fall, yet the incidence of KD continued to rise, both in Japan and here in North America.9 Despite considerable investigative efforts, the cause of KD remains unknown. Recently though, a few tantalizing clues have emerged.
Researchers including Jane Burns, MD, professor in residence at the University of California, San Diego, spotted a trend: Cases were sharply seasonal, peaking in the winter and early spring, and again in early summer, which suggested that an environmental factor could be involved.10 What might that be? Some fairly sophisticated climatological pattern analyses observed that when the dominant jet stream winds blew from central Asia across Japan, the number of Kawasaki’s disease (KD) cases skyrocketed. In fact, all three major outbreaks in Japan had followed this pattern, which was also evident in the normal disease seasons. However, when the winds shifted to blow from the Pacific, the number of cases dropped.11 And when winds from central Asia made their way to Hawaii or California, cases spiked there, too. Although intriguing, this theory remains just that, a theory. For now, the etiology of KD may truly be blowin’ in the wind.
Find That Needle in a Haystack
And then there are those critically ill patients whose fever and accompanying clinical features strongly imply infection but despite countless cultures of various bodily fluids and tissues, there is no confirmation of a cause. These cases often reach an alarming dead end with few remaining viable therapeutic options, especially after multiple antibiotic regimens have failed to provide benefit.
Such was the case recently when our rheumatology consult service—led by one of our intrepid fellows, Kevin Wei, MD, PhD—was helping manage a febrile, middle-aged man with a history of seronegative RA who was experiencing a spiral descent that included worsening heart disease, blood culture negative endocarditis and, to top it off, acute bilateral uveitis, myositis and orchitis. The reams of lab test results led the team nowhere; diagnoses, mostly infectious and autoimmune, were proffered, but despite several courses of empiric antibiotics there were few tangible benefits. A series of heroic cardiac and ophthalmologic surgeries yielded tissue specimens that seemed to be bound by vows of secrecy. Although his excised mitral valve tissue had all the pathological trappings of an infectious endocarditis, all studies, including polymerase chain reaction (PCR) testing, returned negative. A diagnostic cul-de-sac.
When it seemed that every available option had been exhausted, there was just one remaining card to play, the medical equivalent of a Hail Mary football pass. 16S PCR is a novel, costly (approximately $50,00012), new form of metagenomic deep sequencing (MDS) that has been developed based on some of the whirlwind advances in sequencing technology and bioinformatics made in recent years. Literally overnight, MDS has made an unbiased deep sequencing approach an increasingly feasible method for rapidly interrogating all the genetic material contained in a tissue sample.13
The test was worth every penny; the genetic interrogation coaxed the excised heart valve to confess to having been infected with Tropheryma whipplei, that wily and elusive organism best known as the causative agent for the nasty imitator of rheumatologic illness, Whipple’s disease. So much for a prior diagnosis of seronegative RA, which eventually disappeared along with many of his other symptoms following a change in his antibiotic regimen. MDS has helped identify an infectious cause in many cases of meningoencephalitis and uveitis in a timely fashion.14 Long-term harm can be averted. No doubt, we may be hearing more about its potential utility in determining the cause of cerebritis in those situations when the differential diagnosis includes such conditions as Behçet’s disease, lupus or vasculitis.
Hindsight
Many years ago, I was interviewing for a junior faculty position when I was taken aback by the questioning of the interviewer, who wondered aloud why I considered my five years toiling in a laboratory studying immune mechanisms in RA to be a fruitful use of my time. “You would have been better off studying microbiology” was his retort to the look of consternation spreading across on my face. For years, I considered this to have been a flippant remark. Now, I am not so sure.
 Simon M. Helfgott, MD, is associate professor of medicine in the Division of Rheumatology, Immunology and Allergy at Harvard Medical School in Boston.
Simon M. Helfgott, MD, is associate professor of medicine in the Division of Rheumatology, Immunology and Allergy at Harvard Medical School in Boston.
References
- Hair M, Sharpe J (eds). Fast facts about the human microbiome. Center for Ecogenetics & Environmental Health. 2014 Jan.
- Abdollahi-Roodsaz S, Abramson SB, Scher JU. The metabolic role of the gut microbiota in health and rheumatic disease: mechanisms and interventions. Nat Rev Rheumatol. 2016 Aug;12(8):446–455.
- Rascovan N, Duraisamy R, Desnues, C. Metagenomics and the human virome in asymptomatic individuals. Annu Rev Microbiol. 2016 Sep 8;(70):125–141.
- Agnello V, Koffler D, Eisenberg JW, et al. C1q precipitins in the sera of patients with systemic lupus erythematosus and other hypocomplementemic states: Characterization of high and low molecular weight types. J Exp Med. 1971 Sep 1;134(3):228–241.
- Agnello V. The Kunkel legacy and hepatitis C virus infection. Clin Immunol. 2016 Aug 6. pii: S1521-6616(16)30228-5. doi: 10.1016/j.clim.2016.07.023. [Epub ahead of print].
- Amlie-Lefond C, Gilden D. Varicella zoster virus: A common cause of stroke in children and adults. J Stroke Cerebrovasc Dis. 2016 Jul;25(7):1561–1569.
- Gilden D, White T, Khmeleva N, et al. Prevalence and distribution of VZV in temporal arteries of patients with giant cell arteritis. Neurology. 2015 May 12;84(19):1948–1955.
- Kawasaki T. [Acute febrile mucocutaneous syndrome with lymphoid involvement with specific desquamation of the fingers and toes in children]. [article in Japanese]. Arerugi. 1967 Mar;16(3):178–222.
- Frazer J. Infectious disease: Blowing in the wind. Nature. 2012 Apr 4;484(7392):21–23.
- Burns JC, Cayan DR, Tong G, et al. Seasonality and temporal clustering of Kawasaki syndrome. Epidemiology. 2005 Mar;16(2):220–225.
- Rodó X, Ballester J, Cayan D, et al. Association of Kawasaki disease with tropospheric wind patterns. Sci Rep. 2011;1:152–158.
- Wei K. Personal communication.
- Wilson MR, Shanbhag NM, Reid MJ, et al. Diagnosing balamuthia mandrillaris encephalitis with metagenomic deep sequencing. Ann Neurol. 2015 Nov;78(5):722–730.
- Wilson MR, Naccache SN, Samayoa, E et al. Actionable diagnosis of neuroleptospirosis by next-generation sequencing. N Engl J Med. 2014 Jun 19;370(25):2408–2417.


