Overall, high levels of anti-NET antibodies were seen in patients with primary APS and were thought to impair NET clearance and activate the complement cascade, leading to clinical manifestations of APS, including thrombosis. These antibodies may potentially be used to risk-stratify patients with positive aPL antibodies and perhaps be used to determine an indication for primary thrombosis prophylaxis based on thrombotic risk.
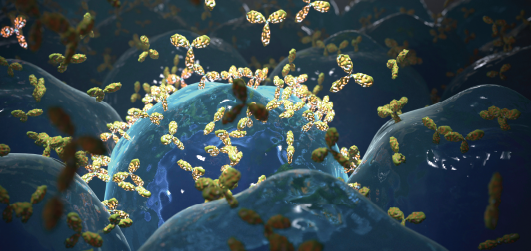
www.sciencephoto.com / shutterstock.com
The Implications
This study identifies potential biomarkers to stratify the risk for primary/secondary autoimmune thrombotic phenomena. Although APS diagnostic criteria are established, appropriate cut-off values for antiphospholipid antibody positivity are debated. In individuals with a clotting history and positive antiphospholipid titers below the APS cut-off values (i.e., <40 units or below the 99th percentile), anti-NET titers and/or NET degradation measurements may serve as additional biomarkers to risk stratify patients who would benefit from anticoagulation. Perhaps individuals without a clotting history, but with anti-NET antibodies, may benefit from prophylactic anticoagulation.
Additionally, the study identifies additional humoral connections to thrombotic phenomena. Thus, B cell therapies, such as rituximab and belimumab, may modulate thrombotic risks in patients with anti-NET antibodies regardless of the presence of antiphospholipid antibodies. Because anti-NET antibody serologies are associated with complement consumption markers, B cell therapies for patients with anti-NET antibodies may ultimately decrease thrombotic risk in diseases mediated by immune complex deposition and complement activation, such as lupus. Alternatively, perhaps anti-NET antibody serologies represent a new pharmacological treatment target.
The NET microenvironment warrants further exploration. Perhaps different antigen-binding sites for anti-NET antibody serologies confer different thrombotic risks. Given that many rheumatic illnesses are associated with increased thrombotic risk, perhaps other autoimmune serologies, such as anti-ds-DNA or anti-CCP, also cross-react with NET antigens to promote thrombotic phenomena.
Given the evolving understanding of the NET microenvironment as it relates to thrombotic pathology, larger studies are needed to confirm the results of this study and better elucidate other thrombotic associations with anti-NET antibody serologies. If the results of this study are reproducible, we anticipate a future in which clinicians may potentially use commercially available anti-NET antibody assays in combination with anti-phospholipid assays to better understand thrombotic risks.
2022 Tournament Chances
Since 2004, NET biology has flourished, and we now know NETs contribute to the pathogenesis of multiple autoimmune conditions. This paper examines a further potential implication of NET dysregulation via anti-NET antibodies on thrombosis generation. Additional studies may further elucidate this finding to potentially equip clinicians with a biomarker to assess thrombotic risk among patients.
