“What can I eliminate from my diet to cure my arthritis?” is the question every client with arthritis asks me. Numerous case reports document patients who achieved lower markers of inflammation and reduced pain and stiffness associated with the removal of one or two food groups from a diet, but historically, no compelling evidence has indicated that what you eat could influence the course of the disease. Therefore, the usual answer has been, “You can eat whatever you want to eat.”
Fast forward to 2025, and you can now find an abundance of articles on nutrition and arthritis. Two main approaches to arthritis and nutrition exist: a whole diet approach vs. a specific foods approach. New avenues being explored include the influence of the gut microbiota and fasting.
Current Research
In the past decade, nutrition research has shifted to focus on a whole-diet approach to managing disease rather than looking for a single food or nutrient as the cause of disease. This is also true for arthritis. There is evidence that following a Mediterranean eating pattern leads to lower levels of disease activity and lower levels of pain and stiffness.1 Another study has shown an anti-inflammatory diet resembling the Mediterranean eating pattern also reduces disease activity.2
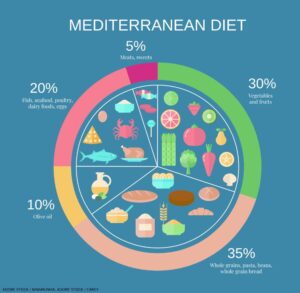
In general, a Mediterranean-style diet has fewer red meats and refined carbohydrates than a typical American diet. It emphasizes fruits and vegetables, whole grains, nuts and legumes, lean meats, fish and healthy fats.
The Mediterranean diet helps reduce disease activity, pain and stiffness by encouraging adequate consumption of various nutrients involved in various pathways that reduce inflammation. Those nutrients include omega-3 fatty acids, vitamin D, minerals and plant nutrients.3-5 At the same time, following the Mediterranean eating pattern leads to a reduction in the consumption of foods believed to increase inflammation and obesity (a separate driver of inflammation): ultra-processed foods, especially sugar, sweetened beverages, sweets and desserts, refined carbohydrates and meat.6,7
Vegan and vegetarian diets have also been studied, but the results are less consistent than a Mediterranean eating plan. This could, in part, be due to study design or to the difficulty some participants have in following these eating patterns because they are very different from the typical North American diet.
Many researchers focus on finding specific foods that cause arthritis. To date, the foods most often investigated are those that contain gluten and dairy products. Many case reports suggest these foods may be involved in development and management of arthritis. However, the evidence remains low grade.
It’s important to note that changes in the gut microbiota have been seen in people with arthritis.8,9 Although it’s not yet clear if pre- and probiotic supplements could treat arthritis, it’s probable that consuming a diet rich in fiber, plant nutrients and fermented foods can improve the diversity and vitality of the gut microbiota and benefit people with arthritis.
Another new avenue of research is fasting. To date, the research is not conclusive, but this may be due, in part, to the fact that many different fasting protocols exist.10
It’s also important to note that following a Mediterranean eating pattern has been linked to maintaining a healthy body weight and to reducing the incidence of heart disease, type 2 diabetes and depression, all of which are comorbidities of arthritis. This information adds weight to the recommendation that your patients adopt this eating pattern.
What’s the Answer?
How can you answer your clients’ questions on diet? First, ask your clients to fill out a validated Mediterranean diet screening questionnaire. If the client is already following the Mediterranean eating pattern, congratulations are in order. Roxanne Bennet and colleagues analyzed data from the Canadian Longitudinal Study on Aging and found that seniors with arthritis were more likely to be at nutritional risk than seniors who do not have arthritis.11 Suggest patients consult with a registered dietitian who can help them better understand what eating habits they currently have and how to use those habits to build a healthier diet.
Second, encourage patients to focus on small nudges instead of a complete diet overhaul. There is evidence these behavioral nudges to routines and habits result in more sustainable changes to diet and health.12
Third, reassure your clients that changing their diet and specifically limiting a single food or food group (e.g., dairy or gluten) may not affect their disease activity or their symptoms. Encourage them instead to try the Mediterranean diet approach. You may also want to consider testing for celiac disease, vitamin D levels and the omega-3 index.
Finally, encourage clients to adopt habits that can improve the health of their gut microbiota. The Mediterranean eating plan is a good place to start, and a meeting with a dietitian can help clients to focus on the appropriate nudges they need to make so they will enjoy the maximum benefit.
 Kim Arrey, DtP, is a preceptor for students in dietetics and a guest lecturer at McGill University, Montreal, for students in dietetics and medicine. She’s also a member of the Ordre des Diététistes Nutritionnistes de Quebec and Dietitians of Canada. A graduate of McGill University, she completed the Certification in Adult Weight Management from the Academy of Nutrition and Dietetics, the Learning Retreat on the Principles of Interdisciplinary Obesity Management for Dietitians, and the Level 1 CHEF Coaching certificate from Harvard University. Ms. Arrey has been a reviewer for Practice-Based Evidence in Nutrition—The Global Resource for Nutrition Practice. She also co-authored The Complete Arthritis Health, Diet Guide and Cookbook.
Kim Arrey, DtP, is a preceptor for students in dietetics and a guest lecturer at McGill University, Montreal, for students in dietetics and medicine. She’s also a member of the Ordre des Diététistes Nutritionnistes de Quebec and Dietitians of Canada. A graduate of McGill University, she completed the Certification in Adult Weight Management from the Academy of Nutrition and Dietetics, the Learning Retreat on the Principles of Interdisciplinary Obesity Management for Dietitians, and the Level 1 CHEF Coaching certificate from Harvard University. Ms. Arrey has been a reviewer for Practice-Based Evidence in Nutrition—The Global Resource for Nutrition Practice. She also co-authored The Complete Arthritis Health, Diet Guide and Cookbook.
References
- England BR, Smith BJ, Baker NA, et al. 2022 American College of Rheumatology Guideline for Exercise, Rehabilitation, Diet, and Additional Integrative Interventions for Rheumatoid Arthritis. Arthritis Care Res (Hoboken). 2023 Aug;75(8):1603–1615.
- Vadell AKE, Bärebring L, Hulander E, et al. Anti-inflammatory diet in rheumatoid arthritis (ADIRA)—A randomized, controlled crossover trial indicating effects on disease activity. Am J Clin Nutr. 2020 Jun 1;111(6):1203–1213.
- Poggioli R, Hirani K, Jogani VG, et al. Modulation of inflammation and immunity by omega-3 fatty acids: A possible role for prevention and to halt disease progression in autoimmune, viral, and age-related disorders. Eur Rev Med Pharmacol Sci. 2023 Aug;27(15):7380–7400.
- Athanassiou L, Kostoglou-Athanassiou I, Koutsilieris M, et al. Vitamin D and autoimmune rheumatic diseases. Biomolecules. 2023 Apr 21;13(4):709.
- Bañuls-Mirete M, Ogdie A, Guma M. Micronutrients: Essential treatment for inflammatory arthritis? Curr Rheumatol Rep. 2020 Oct 26;22(12):87.
- Ma X, Nan F, Liang H, et al. Excessive intake of sugar: An accomplice of inflammation. Front Immunol. 2022 Aug 31;13:988481.
- Li J, Gan Y, Liu J, et al. Red meat intake is associated with early onset of rheumatoid arthritis: A cross-sectional study. Sci Rep. 2021 Mar 11;11(1):5681.
- Zhao T, Wei Y, Zhu Y, et al. Gut microbiota and rheumatoid arthritis: From pathogenesis to novel therapeutic opportunities. Front Immunol. 2022 Sep 8;13:1007165.
- Wang Z, Li Y, Liao W, et al. Gut microbiota remodeling: A promising therapeutic strategy to confront hyperuricemia and gout. Front Cell Infect Microbiol. 2022 Aug 10;12:935723.
- Adawi M, Damiani G, Bragazzi NL, et al. The impact of intermittent fasting (Ramadan fasting) on psoriatic arthritis disease activity, enthesitis, and dactylitis: A multicentre study. Nutrients. 2019 Mar 12;11(3):601.
- Bennett R, Demmers TA, Plourde H, et al. Arthritis is associated with high nutritional risk among older Canadian adults from the Canadian longitudinal study on aging. Scientific Reports. 2024 May 11;14(1):10807.
- Papandreou P, Gioxari A, Daskalou E, et al. Mediterranean diet and physical activity nudges versus usual care in women with rheumatoid arthritis: Results from the MADEIRA randomized controlled trial. Nutrients. 2023 Jan 28;15(3):676.