In the study by Melles and Marmor, doses higher than 5 mg/kg/day had rates of retinal toxicity of 10% within 10 years, which increased further after 20 years to 40%. In contrast, between 4 and 5 mg/kg, the risk was as low as 2% within 10 years and 20% after 20 years.9 This has been reflected in the most recent American Academy of Ophthalmology (AAO) retinal toxicity monitoring recommendations.13 Utilizing real body weight, typically up to a maximum of 400 mg, also has the advantage of being more convenient in the clinic.
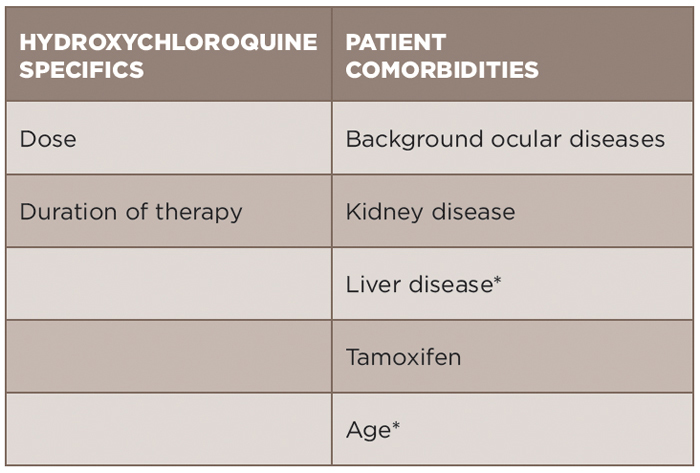
Risk Factors
An individualized approach for assessment of risk of toxicity must be utilized (see Table 1). Age must be considered, in part because ocular diseases that accumulate with age could pose difficulty in terms of monitoring. Hydroxychloroquine is metabolized by the kidney and liver. Kidney disease has been demonstrated to increase the risk of toxicity (odds ratio 2.08) in the most recent study by Melles and Marmor.9 Liver disease in this same study was not identified to be associated with risk, but must be considered due its role in metabolism. Concurrent tamoxifen use has also been identified as a significant risk factor for retinal toxicity (odds ratio 4.59).9 However, blood level monitoring of hydroxychloroquine thus far has not been able to be used in the clinical setting to predict risk for retinal toxicity.2
Genetic factors are also being increasingly evaluated for their association with risk.14 Clinical trials are currently in process to further evaluate the role of genetics and hydroxychloroquine toxicity.
Screening
The American Academy of Ophthalmology (AAO) published updated retinal toxicity monitoring for hydroxychloroquine/chloroquine recommendations in 2016 (see Table 2).13 The dreaded consequence of hydroxychloroquine is “bull’s eye retinopathy,” which results in a ring scotoma. Ideally, earlier changes can be identified to prevent progression to this stage, which emphasizes the importance of screening.
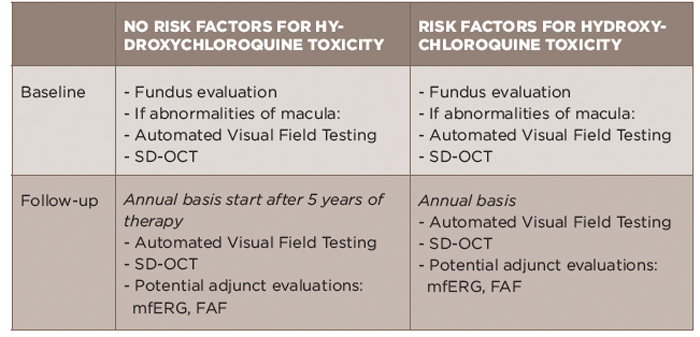
TABLE 2: Summary of 2016 AAO Screening Recommendations for Hydroxychloroquine Toxicity13
AAO: American Academy of Ophthalmology; FAF: fundus autofluorescence; mfERG: multifocal electroretinogram; SD-OCT: spectral domain-optical coherence tomography
The emphasis of baseline testing is the fundus evaluation of the macula. If abnormalities of the macula are noted, AAO would recommend proceeding with baseline visual fields and SD-OCT.13 The visual field testing should take into account a patient’s race/ethnicity as patients with Asian background can have toxicity that is not limited to the macula.15,16