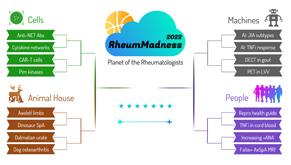
 Editor’s note: RheumMadness is the place for everyone crazy about rheumatology to connect, collaborate, compete and learn together. During RheumMadness, rheumatology concepts represent teams that compete against each other in a tournament, much like basketball teams do in the NCAA’s March Madness tournament. In a series for The Rheumatologist, readers will get a chance to read the scouting reports for each concept team. These reports are written by rheumatology fellows from 13 programs throughout the U.S.
Editor’s note: RheumMadness is the place for everyone crazy about rheumatology to connect, collaborate, compete and learn together. During RheumMadness, rheumatology concepts represent teams that compete against each other in a tournament, much like basketball teams do in the NCAA’s March Madness tournament. In a series for The Rheumatologist, readers will get a chance to read the scouting reports for each concept team. These reports are written by rheumatology fellows from 13 programs throughout the U.S.
Don’t forget to submit your RheumMadness 2022 bracket by March 25. The more your picks match those of our Blue Ribbon Panel of rheumatologists, the more points you get. Learn more about the panel and how the brackets work online.
Connect with RheumMadness by subscribing to the podcast and joining the conversation on Twitter, #RheumMadness. Learn more on the RheumMadness website.
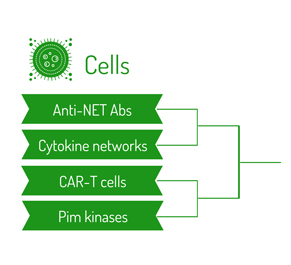
Region: Cells Team: Cytokine Networks
Cytokines are famously confusing for everyone. To illustrate why, try typing the word cytokine into Google images. Without fail, you will find diagrams filled with countless arrows, seemingly illustrating how cytokines go everywhere and do everything in the immune system. It’s tempting to throw up your hands and say, “It’s just too complicated.” However, slowly but surely, the field of rheumatology is making progress in detangling the cytokines web, finding order in the inflammatory mess.
In the base article for this team, researchers from the PRECISE Systemic Autoimmune Diseases (PRECISESADS) collaboration identified a pro-inflammatory cytokine network shared by four rheumatic conditions: systemic lupus erythematosus (SLE), Sjögren’s syndrome, rheumatoid arthritis (RA) and systemic sclerosis (SSc).1 This cytokine network is defined primarily by elevations in CXCL10, interleukin (IL) 2, IL-6 and tumor necrosis factor (TNF).
 Intriguingly, patients with the highest levels of this pro-inflammatory cytokine profile have more severe clinical manifestations, regardless of their underlying diagnosis. Example: This cytokine network is associated with kidney involvement in SLE; extra-glandular manifestations in Sjögren’s syndrome; and pulmonary, renal or vascular manifestations in SSc.
Intriguingly, patients with the highest levels of this pro-inflammatory cytokine profile have more severe clinical manifestations, regardless of their underlying diagnosis. Example: This cytokine network is associated with kidney involvement in SLE; extra-glandular manifestations in Sjögren’s syndrome; and pulmonary, renal or vascular manifestations in SSc.
The investigators also demonstrated unique associations between this pro-inflammatory cytokine network and alterations in key immune cell populations (e.g., plasmablasts, memory B cells, etc.) in each condition.
Finally, the researchers explored how this inflammatory cytokine network may participate in the communication between B and T cells through a variety of co-culture experiments in vitro.
Just like cytokines themselves, the base article for this team is complex. However, the overall message is one of simplicity, showing how cytokine networks can unify disparate rheumatic diseases through shared pathogenic mechanisms.
Implications
In 2013, Schett et al. published a prescient review in Nature Medicine, noting the startling success of targeted cytokine inhibitors in the 1990s “indicates that chronic inflammatory diseases depend on fragile communication networks of cytokines, which collapse upon neutralization of functionally vulnerable nodes, such as TNFα.”2
Indeed, rheumatologists now think in terms of cytokine networks on a daily basis. You say gout? We think IL-1. Psoriatic arthritis? TNFα, IL-17, IL-12/23 and Janus kinase immediately come to mind. What about IBD-arthritis? Same list, omitting IL-17. Cytokine networks are becoming so second nature to rheumatologists that we can’t help but dream of a day when we can drop broad immunosuppressants almost entirely. (We’re looking at you, GUSTO [giant cell arteritis treatment with ultra-short glucocorticoid and tocilizumab].3)
With this background in mind, the base article for this team advances our understanding of cytokines by studying the cytokine profiles of four different rheumatic diseases all at once, ultimately describing a shared cytokine network particularly active in patients with severe disease. Besides the obvious implications for future drug development, this study raises an interesting question for current and future researchers: What other cytokine networks are waiting to be described if the same methodology is applied to other groups of rheumatic diseases? If you could choose another group of four conditions to put into this cytokine network detangler machine, what would they be? Will studies using the methodology in PRECISESADS eventually allow us to redefine rheumatic diseases by shared and unique pathophysiology rather than clinical manifestations alone?
Chances in the Tournament
In our view, this team’s chances in the tournament depend on how narrowly or broadly the Blue Ribbon Panel views the concept of cytokine networks in rheumatology. The base article for this team uses a complex, sophisticated playbook to describe a shared pro-inflammatory cytokine network in four rheumatic conditions. Although this fact will certainly score some points with the panel, it may not be enough for the team to escape its first-round matchup against the upstart anti-NET antibodies. However, the panel may apply the concept of cytokine networks more broadly, viewing the base article as a crucial piece in the massive cytokine jigsaw puzzle that is continually revolutionizing our understanding of disease pathogenesis and therapeutic targets in rheumatology. If that’s the case, this team may be cutting down the nets at the end of the tournament. Surrounded, of course, by a cloud of cytokine confetti.
David Leverenz, MD, is assistant professor of medicine at Duke University School of Medicine, Durham, N.C.
Akrithi Udupa, MD, is assistant professor of medicine at MedStar Georgetown University Hospital, Washington, D.C.
Guy Katz, MD, is a second-year rheumatology fellow at Massachusetts General Hospital, Boston.
Lauren He, MD, is an internal medicine resident at the University of Chicago School of Medicine.
Ben Kellog, MD, is an internal medicine resident at Duke University School of Medicine, Durham, N.C.
Michael Macklin, MD, is an internal medicine resident at the University of Pittsburgh Medical Center.
Courtney Bair is a medical student at Duke University School of Medicine, Durham, N.C.
Matthew Sparks, MD, is an associate professor of medicine at Duke University School of Medicine, Durham, N.C.
Lisa Criscione-Schreiber, MD, MEd, is a professor of medicine at Duke University School of Medicine, Durham, N.C.
References
- Simon Q, Grasseau A, Boudigou M, et al. A proinflammatory cytokine network profile in Th1/type 1 effector B cells delineates a common group of patients in four systemic autoimmune diseases. Arthritis Rheumatol. 2021Aug;73(8):1550–1561.
- Schett G, Elewaut D, McInnes IB, et al. How cytokine networks fuel inflammation: Toward a cytokine-based disease taxonomy. Nat Med. 2013 Jul;19(7):822–824.
- Christ L, Seitz L, Scholz G, et al. EULAR. A proof-of-concept study to assess the efficacy of tocilizumab monotherapy after ultra-short glucocorticoid administration to treat giant cell arteritis—the GUSTO trial [abstract OP0061]. Ann Rheum Dis. 2021 Jul;80(suppl 1):33.
 Experience All of RheumMadness
Experience All of RheumMadness
During RheumMadness, rheumatology concepts represent teams that compete against each other in a tournament, much like basketball teams do in the NCAA’s March Madness tournament. In a series for The Rheumatologist, readers will get a chance to read the scouting reports. Check out the reports from each region:
Region: Cells
Region: Animal House
Region: Machines
Region: People
• False Positive MRI in Axial SpA
Don’t forget to submit your RheumMadness 2022 bracket by March 25. The winner of each match-up is decided by a seven-member Blue Ribbon Panel of rheumatologists. The panel will vote based on which topic they think is most important to patients, providers and researchers—both now and in the future. The more your picks match those of the panel, the more points you get. The tournament results will be released in four rounds from March 26–April 4. Prizes will be given to participants with the top scores in the following categories: 1) attending/APP, 2) fellow and 3) resident/medical student. The prize is a custom RheumMadness coffee mug and a lifetime of bragging rights.
Connect with RheumMadness by subscribing to the podcast and joining the conversation on Twitter, #RheumMadness. Learn on the RheumMadness website.