It’s important to be able to identify and perform intensive, deep phenotyping of people who are both antibody positive and genetically at risk in order to one day intervene early, before inflammation can begin to damage joints, and to improve therapies, he said.
The lungs are a good place to look for clues that a person may be at risk for RA. Lung disease is associated with elevations of RA-related, anti-CCP3.1 autoantibodies, and smoking tobacco and breathing silica particulate matter are two risk factors for RA, Dr. Holers noted.
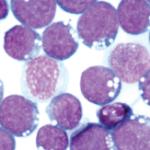
In one paper published in Arthritis & Rheumatology in 2014, researchers described the results of DNA barcoding to sequence antibodies expressed by plasmablasts in the blood serum of RA patients, he said. Their analysis results of isotype frequencies in this population showed a dramatic skewing to IgA, antibodies that are largely found in mucosal surfaces such as the linings of the lungs.
“There is increasing evidence that mucosal inflammation is driving this disease,” said Dr. Holers. Whether in gingivitis, periodontitis or pulmonary disease, the original sin’s trail may begin on mucosal surfaces.
But how do genes come into play? “We are on the road to understanding genetics, but we still don’t know how many genetic factors are involved in each phase of this disease,” said Dr. Holers. “We know some of the fundamental principles, such as that genes play a role in the high affinity for ACPA responses in these individuals, specifically in the preclinical period.”
Susan Bernstein is a freelance medical journalist based in Atlanta.
Second Chance
If you missed this session at the 2015 ACR/ARHP Annual Meeting, it’s not too late. Catch it on SessionSelect.