Editor’s Note: This article initiates a new department in The Rheumatologist that will focus on regional musculoskeletal disorders that may be seen by both rheumatologists and orthopedic surgeons. To promote the care of these patients and facilitate communication between rheumatologists and orthopedists, these articles will provide focused discussions of clinical and radiographic findings and describe management principles from the orthopedic perspective. We hope that this series will increase awareness of the diversity and complexity of painful musculoskeletal conditions and enhance patient outcomes through improved collaboration between medical and surgical specialists.


Meniscus Extrusion
Meniscus extrusion is a common, but often overlooked, source of joint line pain that can be associated with knee arthritis. An extrusion occurs when the meniscus subluxates out of the tibiofemoral joint into the adjacent gutter. A meniscus is at risk for extrusion when there is arthritis in its compartment and when pathology of the meniscus, particularly a tear, can weaken its structure.
Meniscus extrusion is a condition important for rheumatologists to consider as they evaluate patients with knee pain because of the important implications for prognosis and management. Most patients with a symptomatic extrusion present with joint line pain and radiographs show narrowing of the joint space. This presentation is difficult to separate from osteoarthritis (OA) or inflammatory arthritis alone and patients are often managed with medications and physical therapy/exercise. Because meniscus extrusion can be a harbinger of rapidly progressive arthritis in the affected compartment, recognizing an extrusion should trigger aggressive preventative measures, particularly in the young to middle-aged patient. In addition, the extruded meniscus is a painful entity that may benefit from arthroscopic surgery.
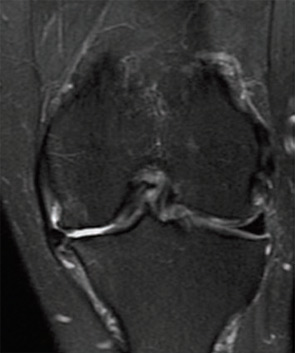
Meniscus extrusion is measured in millimeters from the most peripheral aspect of the tibial plateau, excluding any osteophytes, to the peripheral edge of the extruded meniscus in the midline of the joint.1 This distance is measured on coronal MRI images (see Figure 1, below left). Subluxation of the meniscus more than 3 mm is significantly associated with the extent of meniscal degeneration, extent of meniscus tear, complex tears, large radial tears, and tears involving the meniscal root.2 Severe degrees of subluxation (>7 mm) are strongly correlated with severity of medial joint space narrowing and the presence of symptomatic osteoarthritis (OA).3 Extrusion occurs more frequently on the medial side of the knee than the lateral side.
When a meniscus extrusion is symptomatic, patients often report joint line pain that is severe, constant, worse with weight bearing, and when medial, the patient often has to sleep with a pillow between the knees to limit contact. On examination, the affected joint line may appear swollen and the joint line and adjacent femur and tibia are exquisitely tender, particularly along the mid and anterior portion of the joints.
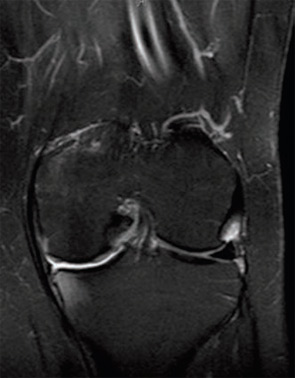
Plain radiographs of a knee with a meniscus extrusion demonstrate narrowing of the joint space with or without osteophytes and flattening of the femoral condyle and squaring and sclerosis of the tibial plateau. On MRI, the extruded meniscus may be displaced superiorly or inferiorly in the medial or lateral gutters. Frequently, MRI shows adjacent edema in the medial collateral ligament (MCL) and its bursa medially (see Figure 1, left). This MCL edema may be due to several factors including the pressure of the extruded meniscus on the local capsule and ligament, inflammation of the synovio-entheseal complex, local friction from osteophytes against the MCL during knee movement, and increased force upon the MCL due to changes in knee mechanics (increased load transmission, loss of shock absorption, and decreased congruency of the femorotibial joint) caused by the meniscal extrusion.4-7 MRI frequently demonstrates bone marrow edema in the femoral condyle and tibial plateau adjacent to the extruded meniscus (see Figure 2B, above). It is worth noting that bone marrow edema is also a risk factor for rapid structural deterioration in knee osteoarthritis; its relation to progression may be explained in part by its association with limb malalignment.8-10
Determining whether a patient has a symptomatic extrusion of the meniscus, rather than arthritis alone, has important implications for treatment. The extruded meniscus may not improve with typical non-operative treatments for arthritis, such as physical therapy and exercise, corticosteroid injections, or other medications. More aggressive treatment can be considered to improve the biomechanical environment in the affected compartment. Unloader braces may help pain by decreasing mechanical stress by reducing malalignment and improving joint stability.11 The use of bisphosphonates to treat bone marrow edema and perhaps to decrease subchondral bone turnover associated with OA can be considered, although this approach is controversial.12
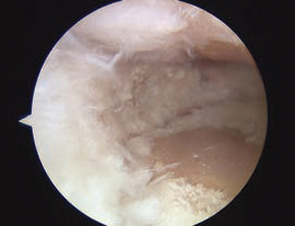
Arthroscopic surgery has a place in managing the arthritic knee with a symptomatic meniscus extrusion. While arthroscopic surgery may be controversial for the treatment of arthritis in general (i.e., lavage alone for relief of pain), surgery remains beneficial for treating mechanical symptoms associated with meniscus tears, delaminating chondral lesions and loose bodies. In the case of a meniscus extrusion, arthroscopic meniscus debridement may provide relief by decreasing impingement of the thickened, extruded meniscus upon local structures such as the MCL (see Figure 2, above).
In summary, meniscus extrusion may occur with symptomatic knee arthritis, especially when radiographs show advanced joint space narrowing. Extrusion may be treated differently than arthritis alone, especially in the young or middle-aged patient who is not yet a candidate for arthroplasty.
Dr. Toth is director of the Women’s Sports Medicine Program and assistant professor of orthopaedic surgery at Duke University Medical Center in Durham, N.C.
References
- Breitenseher MJ, Trattnig S, Dobrocky I, et al. MR imaging of meniscal subluxation in the knee. Acta Radiol. 1997; 38:876-879.
- Costa CR, Morrison WB, Carrino JA. Medial meniscus extrusion on knee MRI: Is extent associated with severity of degeneration or type of tear? Am J Roentgenol. 2004;183:17-23.
- Gale DR, Chaisson CE, Totterman SM, Schwartz RK, Gale ME, Felson D. Meniscal subluxation: Association with osteoarthritis and joint space narrowing. Osteoarthritis Cartilage. 1999;7:526-532.
- Wen DY, Propeck T, Kane SM, Godbee MT, Rall KL. MRI description of knee medial collateral ligament abnormalities in the absence of trauma: Edema related to osteoarthritis and medial meniscal tears. Magn Reson Imaging. 2007;25:209-214.
- McGonagle D, Lories RJ, Tan AL, Benjamin M. The concept of a “synovio-entheseal complex” and its implications for understanding joint inflammation and damage in psoriatic arthritis and beyond. Arthritis Rheum. 2007;56:2482-2491.
- Bergin D, Keogh C, O’Connell M, Rowe D, Shah B, Zoga A, Fitzpatrick P, Eustace S. Atraumatic medial collateral ligament oedema in medial compartment knee osteoarthritis. Skeletal Radiol. 2002;31:14-18.
- Blankenbaker DG, De Smet AA, Fine JP. Is intra-articular pathology associated with MCL edema on MR imaging of the non-traumatic knee? Skeletal Radiol. 2005;34:462-467.
- Hunter DJ, Zhang Y, Niu J, et al. Increase in bone marrow lesions associated with cartilage loss. Arthritis Rheum. 2006;54:1529-1535.
- Scher C, Craig J, Nelson F. Bone marrow edema in the knee in osteoarthrosis and association with total knee arthroplasty within a three-year follow-up. Skeletal Radiol. 2008; 37:609-617.
- Felson DT, Chaisson CE, Hill CL, et al. The association of bone marrow lesions with pain in knee OA. Ann Intern Med. 2001;134:541-549.
- Brouwer RW, Jakma TS, Verhagen AP, Verhaar JA, Bierma- Zeinstra SM. Braces and orthoses for treating osteoarthritis of the knee. Cochrane Database Syst Rev. 2005; 25(1): CD004020.
- Saag KG. Bisphosphonates for osteoarthritis prevention: “Holy Grail” or not? Ann Rheum Dis. 2008;67:1358-1359.
