The cardiologists’ suggestion that high-dose aspirin be administered alone as first-line therapy for patients with pain and arthritis might have been true as a recommendation 40 years ago, but I would venture to say that there are few—if any—rheumatologists today who use full doses of aspirin as primary therapy for osteoarthritis.
Source:
ACR Subcommittee on OA Guidelines.
Arthritis Rheum. 2000; 43:1905-1915.
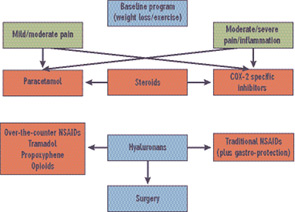
With respect to guidelines for treating OA, the importance of risk versus benefit is, without question, always an uppermost consideration. Unfortunately, pain itself is a cardiovascular risk factor related to increased blood pressure and pulse rate, so lack of pain relief can put the patient at increased risk. Treatment paralysis is not an attractive alternative. Risks of any type are not to be considered lightly, and need to be balanced against relief of pain and improved quality of life—not always an easy decision. Judgment calls by both the patient and physician are important in determining eventual management in any given individual.
Other agents utilized in the symptomatic treatment of osteoarthritis include intra-articular corticosteroids and intra-articular hyaluronans.11 These have the advantage of minimal systemic effects, and are of particular benefit when one or two joints do not respond adequately to other forms of management. At this time, hyaluronans are indicated only for use in osteoarthritis of the knee; they can be considered for use off-label in other joints if appropriate. I have used them in ankle OA with success, and efficacy in OA of the shoulder has been reported. Pre-approval for insurance coverage is recommended.
Glucosamine and chondroitin sulfate have been recommended in the treatment of OA, particularly the knee.12-14 A large study carried out under the auspices of the National Institute of Arthritis and Musculosleletal and Skin diseases and the National Center for Complementary and Alternative Medicine showed that, in a post-hoc hypothesis-testing analysis, a combination of glucosamine and chondroitin sulfate appeared to be effective in individuals with higher degrees of OA pain.15 Based on clinical studies and experience with OA patients, I recommend use of glucosamine and chondroitin sulfate as adjunctive therapy in management.
Other modalities of therapy may be considered in the overall therapeutic approach. Acupuncture has been shown to be effective in the treatment of OA of the knee, although the effect size is low in most individuals. The increased interest in alternative therapies such as tai chi and yoga has led to increased research in evaluating these techniques. Although some studies support efficacy, investigations utilizing larger numbers of subjects in double-blinded studies would add to our knowledge in this arena.
Disease Modification
The elusive target of osteoarthritis management is disease modification with prevention of OA onset or (probably more achievable) retardation of disease progression. At this time, there are no specific agents approved for disease modification. Some studies do suggest that certain agents are associated with a slowing of disease progression, including glucosamine sulfate, chondroitin sulfate, sodium hyaluronan, soybean-avocado extract, and diacerrein.16 Identification of drugs as structure modifying is particularly challenging given that there is disagreement as to the best outcome measure for defining such structure modification. Classically, a slowing of joint-space narrowing (a measure of cartilage loss) has been the gold standard for demonstrating inhibition of disease progression. MRI will detect structural changes earlier and more comprehensively than radiologic study of joint-space narrowing alone.17

