Over the past decade and a half, cross-disciplinary research in immunology and bone biology has led to a revised picture for patients with rheumatoid arthritis. Pivotal work in the late 1990s to early 2000s demonstrated that, as in skeletal bone, osteoclasts were responsible for the destruction of articular bone—and that products of T cells and synovial fibroblasts, such as the receptor activator of ligand (RANKL), were of critical importance in inducing osteoclastogenesis in this setting.1-4 This knowledge, coupled with the rise of effective biologic agents to block inflammatory cytokines, has revolutionized what clinicians can offer to patients to arrest joint erosion.

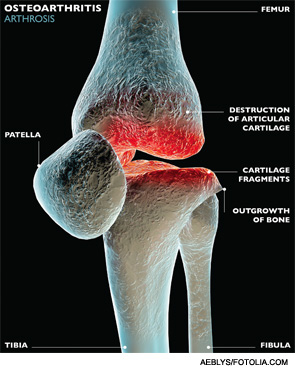
However, many questions remain to be answered for patients with rheumatoid arthritis and the more common joint disease, osteoarthritis. Why do some patients respond to anti-TNF agents while others do not? Does absence of inflammation always connote cessation of structural damage? Might there be an inflammatory component to development of osteoarthritis, despite the perception that it’s a degenerative process? Will an understanding of bone-immune system signaling lead to ways to induce bone repair?
Discoveries about the cross-talk between bone and the immune system in the burgeoning field of osteoimmunology may hold the key to these and other questions, and the development of more tools to address the disease process in other arthritides, according to researchers with whom we spoke.
“Our treatment of this disease [rheumatoid arthritis] is so much better than when I was a trainee that it is quite remarkable,” says Mary Nakamura, MD, PhD, UCSF School of Medicine, San Francisco, who heads osteoimmunology research in the Division of Rheumatology. But, she notes, “that success has made us want to go further, because we know that these treatments do not help everyone.”
The heterogeneity of the disease calls out for better definition of disease subtypes, she says. One current project in Dr. Nakamura’s lab, in concert with Elizabeth Mellins, MD, professor of pediatrics, Stanford (Calif.) School of Medicine, involves profiling patients’ peripheral monocyte white blood cells to determine whether they reflect singular cytokine signatures. Discerning separate subtypes of disease could lead to the development of better biomarkers to predict response to therapy. “There are many choices [of therapies] now, and yet we still have no clearer ability of how to a priori choose between them,” Dr. Nakamura says.