Over the past decade and a half, cross-disciplinary research in immunology and bone biology has led to a revised picture for patients with rheumatoid arthritis. Pivotal work in the late 1990s to early 2000s demonstrated that, as in skeletal bone, osteoclasts were responsible for the destruction of articular bone—and that products of T cells and synovial fibroblasts, such as the receptor activator of ligand (RANKL), were of critical importance in inducing osteoclastogenesis in this setting.1-4 This knowledge, coupled with the rise of effective biologic agents to block inflammatory cytokines, has revolutionized what clinicians can offer to patients to arrest joint erosion.

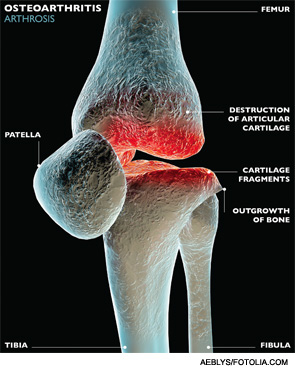
However, many questions remain to be answered for patients with rheumatoid arthritis and the more common joint disease, osteoarthritis. Why do some patients respond to anti-TNF agents while others do not? Does absence of inflammation always connote cessation of structural damage? Might there be an inflammatory component to development of osteoarthritis, despite the perception that it’s a degenerative process? Will an understanding of bone-immune system signaling lead to ways to induce bone repair?
Discoveries about the cross-talk between bone and the immune system in the burgeoning field of osteoimmunology may hold the key to these and other questions, and the development of more tools to address the disease process in other arthritides, according to researchers with whom we spoke.
“Our treatment of this disease [rheumatoid arthritis] is so much better than when I was a trainee that it is quite remarkable,” says Mary Nakamura, MD, PhD, UCSF School of Medicine, San Francisco, who heads osteoimmunology research in the Division of Rheumatology. But, she notes, “that success has made us want to go further, because we know that these treatments do not help everyone.”
The heterogeneity of the disease calls out for better definition of disease subtypes, she says. One current project in Dr. Nakamura’s lab, in concert with Elizabeth Mellins, MD, professor of pediatrics, Stanford (Calif.) School of Medicine, involves profiling patients’ peripheral monocyte white blood cells to determine whether they reflect singular cytokine signatures. Discerning separate subtypes of disease could lead to the development of better biomarkers to predict response to therapy. “There are many choices [of therapies] now, and yet we still have no clearer ability of how to a priori choose between them,” Dr. Nakamura says.

“We understand that many of the pathways by which immune cells ‘talk’ to other cells are potentially used by bone cells to talk to one another,” says Antonios O. Aliprantis, MD, assistant professor of medicine, and director of the Brigham and Women’s Osteoarthritis Center, Boston. “It follows, then, that if we could find these molecules that either bone cells use to talk to one another or immune cells use to talk to bone cells, we may be able to find new potential targets.”
Pivotal Work by Pioneers
The first milestone in understanding the structural damage in RA came in 1998 with the publication of a paper by Ellen M. Gravallese, MD, Steven Goldring, MD, and colleagues, in which they showed definitively the presence of osteoclasts at the pannus–bone interface in the joints of RA patients.1 In 1984, Bromley and Wooley had described TRAP-positive multinucleated cells, a marker of osteoclasts, in tissue sections from patients with RA, but the real wave of knowledge reached critical mass with the advent of modern scientific techniques.5
Dr. Gravallese, currently the Myles J. McDonough Chair in Rheumatology, University of Massachusetts Medical School, Worcester, Mass., recalls, “The rheumatology community was initially skeptical of the importance of our findings, so we felt it was essential to try to understand the pathways driving the differentiation of osteoclasts at these sites.” Dr. Gravallese and colleagues, in collaboration with Christophe Benoist, MD, PhD, professor of microbiology and immunobiology at Harvard Medical School, Boston, showed the link between RANKL, osteoclastogenesis and bone erosion by inducing inflammatory arthritis in RANKL knockout mice and demonstrating that these mice were protected from articular bone loss.2 In parallel experiments, Georg Schett, MD, PhD, Kurt Redlich, MD, and colleagues from the Medical University and the Institute of Molecular Pathology in Vienna, Austria, and the University of Athens (Georg Kollias, PhD), showed that in a different osteoclast-deficient mouse, the c-Fos-deficient mouse, articular bone was also protected from erosion in a TNF-driven arthritis model.3
‘We are beginning to understand that there is an inflammatory component to osteoarthritis.’
In addition, in the late 1990s, the orthopedist/immunologist Hiroshi Takayanagi and colleagues found that synovial macrophages were capable of differentiating into osteoclasts, and posited that this was likely contributory to the bone erosion seen in RA.6 Dr. Takayanagi’s group has also made additional major contributions to this area of investigation.
Drs. Gravallese and Schett now reflect that it has been surprising what a change these initial discoveries have made in what is now the cross-disciplinary field of osteoimmunology. The term osteoimmunology has been attributed to Yongwon Choi, PhD, an immunologist who provided the RANKL knockout mouse used in Dr. Gravallese’s 2000 study. When Dr. Choi initially generated the RANKL knockout mouse, he had identified RANKL as a factor augmenting the interactions between dendritic cells and T cells. When the role of RANKL in osteoclastogenesis was also identified, Dr. Choi is reported to have said, “I was an immunologist, and now I’m an osteoimmunologist.’” The term stuck, and the cross-disciplinary field had a new name.

Dr. Schett, who heads the Department of Internal Medicine and Institute for Clinical Immunology, University of Erlangen-Nuremberg, Erlangen, Germany, has made, in concert with his colleagues, seminal contributions to the field of osteoimmunology. He points out that rheumatoid arthritis has become “a very good clinical example of the interaction between the immune system and the bone.”
Possible to Promote Repair?
Studying the mechanisms of the immune response has led to identification of immune system products that are either cell-surface bound or secrete molecules that can be targeted by monoclonal antibodies or receptor antagonists, with resulting success in blocking the inflammatory response that triggers osteoclastogenesis.7
Although the success of biologic agents to halt bone erosion has been huge, it’s now clear that there is a missing piece to the puzzle, says Dr. Gravallese.
“When we stopped the progression of bone loss in RA patients, I expected that we would see repair of the existing erosions. But that is not the case: After therapeutic intervention, the X-ray [of the bone erosions] typically looks the same, with only limited evidence of repair. We are very interested in the reasons that the bone does not fill in. We have demonstrated that inflammation affects osteoblasts as well as osteoclasts.”
We now know, says Dr. Aliprantis, that “immune system inflammation definitely drives bone loss by activating RANK ligand and osteoclasts and also probably decreases osteoblast function.”

Dr. Schett and his colleagues have conducted several longitudinal studies of patients treated with the current cytokine blockers, and have found some incomplete repair at erosion sites. However, he notes, “Cytokine inhibitors neutralize osteoclast differentiation, but they also blunt new bone formation.”
Julia Charles, MD, PhD, instructor in medicine, Rheumatology Division, Brigham and Women’s Hospital, Boston, and co-author with Dr. Aliprantis of a 2014 paper, “Osteoclasts: More than ‘bone eaters,’”8 adds that evidence from both genetic and in vitro biochemical studies shows that osteoclasts produce substances referred to as “clastokines” that may promote osteoblast recruitment or differentiation. Learning how to leverage these clastokines could result in the Holy Grail—to find an agent that promotes bone formation by osteoblasts and decreases bone resorption at the same time.
Several approaches to repair have been and continue to be explored. Early on, Dr. Redlich, who is now associate professor at the Division of Rheumatology of the Medical University of Vienna, also showed, in another animal model, that combining an anti-TNF agent with administration of teriparatide, a parathyroid hormone used to treat bone loss in osteoporosis, worked to arrest erosion and induce bone repair.9 Dr. Redlich also sees promise in deciphering T cell trafficking to the joints. “Targeting different cell populations selectively in the joint should be our scope for the future,” he says.

Dr. Gravallese, Dr. Schett and others have also shown that inflammation plays a role in inhibiting the osteoblast differentiation and function and that the Wnt/beta-catenin pathway in osteoblasts may be a potential target for inducing bone formation. Based on his group’s preclinical studies, Dr. Schett believes that antibodies against sclerostin may allow repair of existing damage. This line of investigation is now leading these groups onto the next horizon: understanding the mechanisms by which excess bone is made in the entheses, leading to the rigidity and morbidity seen in spondyloarthropathy.
Role of Inflammation in OA?
Although osteoarthritis has generally been perceived as a degenerative disease, “We are beginning to understand that there is an inflammatory component to osteoarthritis,” notes Dr. Aliprantis. “It is more likely to be that some of the degradation products activate macrophages or other innate immune cells to make inflammatory cytokines, which in turn causes more cartilage damage.”

The interplay between the immune system and cartilage is not well understood, he says, but evidence of upregulation of inflammatory pathways was found by his group in the joint fluid of patients with osteoarthritis, which suggests that there is activation of inflammation.10
The role of inflammation in osteoarthritis is one line of investigation at the UCSF/Stanford Arthritis Center of Excellence, funded in part by the Great West Region of the Arthritis Foundation. Dr. Nakamura is the director of the UCSF component of that center, and William Robinson, MD, who has conducted animal studies in this regard, serves as director for the Stanford component. In addition, Mark Genovese, MD, is currently conducting a human trial of OA with hydroxychloroquine and atorvastatin.
Future Horizons
Many challenges remain in osteoimmunology, and worldwide the research activity has increased exponentially. Basic science research by Ellen Gravallese, Georg Schett, Kurt Redlich, Hiroshi Takayanagi, Steven Goldring, Mary Nakamura, Tony Aliprantis and others continues to push the field forward.
Josef Smolen, MD, who is chair of the Division of Rheumatology at the Medical University of Vienna in Austria and chair of the second department of medicine at the Center for Rheumatic Diseases at Hietzing Hospital in Vienna, points out that despite the progress with biologic agents, “erosions by themselves will not affect physical function nearly as much as cartilage damage, which is really the driver of physical function. There is a lot to do in the respect of not only interfering with damage, but in getting repair going. At the end of the day, what we need to look at is the whole gestalt of the joint. Stopping erosions will not be enough if cartilage damage continues to progress.”
As new discoveries unfold, maintaining the communication lines between the bench and the bedside will be key, says Dr. Nakamura.
As to the value of following basic research, Dr. Charles believes that understanding basic biology of the bone and the immune system linkage is “extraordinarily important for us as a community. The basic science mouse-model level, the human translational science level and the clinical trial level: all are important parts of the scientific enterprise. Understanding basic pathophysiology and mechanisms helps us understand new clinical findings, while unexpected clinical findings can and should send us back to the bench to explore new areas of research.”
Gretchen Henkel is a medical journalist based in California.
References
- Gravallese EM, Harada Y, Wang JT, et al. Identification of cell types responsible for bone resorption in rheumatoid arthritis and juvenile rheumatoid arthritis. Am J Pathol. 1998 Apr;152(4):943–951.
- Pettit AR, Ji H, von Stechow D, et al. TRANCE/RANKL knockout mice are protected from bone erosion in a serum transfer model of arthritis. Am J Pathol. 2001 Nov;159(5):1689–1699.
- Kong YY, Yoshida H, Sarosi I, et al. OPGL is a key regulator of osteoclastogenesis, lymphocyte development and lymph-node organogenesis. Nature. 1999 Jan 28;397(6717):315–323.
- Redlich K, Hayer S, Ricci R, et al. Osteoclasts are essential for TNA-alpha-mediated joint destruction. J Clin Invest. 2002 Nov;110(10):1419–1427.
- Bromley M, Woolley DE. Chondroclasts and osteoclasts at subchondral sites of erosion in the rheumatoid joint. Arthritis Rheum. 1984 Sep;27(9):968–975.
- Takayanagi H, Oda H, Yamamoto S, et al. A new mechanism of bone destruction in rheumatoid arthritis: Synovial fibroblasts induce osteoclastogenesis. Biochem Biophys Res Commun. 1997;240(2):279–286.
- Schett G, Gravallese E. Bone erosion in rheumatoid arthritis: Mechanisms, diagnosis and treatment. Nat Rev Rheumatol. 2012 Nov;8(11):656–664.
- Charles JF, Aliprantis AO. Osteoclasts: More than ‘bone eaters.’ Trends Mol Med. 2014 Aug;20(8):449–459.
- Redlich K, Görtz B, Hayer S, et al. Repair of bone erosions and reversal of systemic bone loss upon therapy with anti-tumor necrosis factor in combination with osteoprotegerin or parathyroid hormone in tumor necrosis factor-mediated arthritis. Am J Pathol. 2004 Feb;164(2):543–555.
- Ritte SY, Subbaiah R, Bebek G, et al. Proteomic analysis of synovial fluid from the osteoarthritic knee: Comparison with transcriptome analyses of joint tissues. Arthritis Rheum. 2013 Apr;65(4):981–992.