whitehoune/shutterstock.com
WASHINGTON, D.C.—Successful management of pain remains a challenge for rheumatologists. Five research abstracts presented at the 2016 ACR/ARHP Annual Meeting in a session titled Pain—Basic and Clinical Aspects offered new insights on pain sensitization, and the risks and effects of various pain therapies.
Knee Pain After Surgery
Can we predict which patients will have longer-term pain after total knee arthroplasty (TKA)? The study, “Post-Arthoplasty Pain Trajectories After Total Knee Arthroplasty and Their Association with 6- and 12-Month Pain,” looked at possible associations between early, postsurgical pain trajectories and lingering pain, said lead author Jasvinder A. Singh, MD, MPH, professor of rheumatology and clinical immunology at the University of Alabama, Birmingham.1
Although TKA usually is effective at treating pain and function problems, “about 15% of patients who undergo TKA have residual, moderate-to-severe joint pain that persists two to five years after the procedures,” said Dr. Singh.2 “Our thinking was that pain trajectories may be important. We wanted to look at them to understand what to expect in the future.”
Data from the Function and Outcomes Research for Comparative Effectiveness in Total Joint Replacement and Quality Improvement (FORCE-TJR) database, a nationwide cohort of 28,000 U.S. patients undergoing TKA, was used for the study. First, researchers assessed pain severity on a scale of 0–10 for 659 patients at two and eight weeks after surgery. Participants were 64.5% female and 66.5% age 65 or older. Two pain trajectories were evident: 72% were pain responders, or their pain decreased meaningfully after TKA; 28% were nonresponders.
‘After 12 weeks of DMARD treatment, regional cerebral blood flow in the hand pain condition decreased to levels similar to that of the controls.’ —Dr. Lee
Using patient-reported Knee Injury and Osteoarthritis Outcome Scores (KOOS), “pain trajectories at eight weeks were statistically significantly and clinically meaningfully associated with KOOS scores at six and 12 months,” said Dr. Singh. In KOOS, zero represents extreme knee pain or problems; 100 signifies no pain or problems. Mean KOOS scores for fast pain responders were 87.3 at six months and 90.2 at 12 months, said Dr. Singh. Slow responders’ mean KOOS scores at six months were 74.5 and at 12 months were 77.7. Charlson Comorbidity Count 3, and preoperative physical and mental health scores were also significantly associated with six- and 12-month pain outcomes, he said.
Intervening early to treat postoperative pain may lead to better outcomes, although “this study did not collect pain data during the inpatient stay, or the first week after TKA, which may be the most important time,” said Dr. Singh.
Why Some Pain Persists
Lower levels of pain sensitization in patients with osteoarthritis (OA) are associated with lower levels of progression to constant pain, according to “Relation of Pain Sensitization to the Evolution from Intermittent to Chronic, Persistent Pain in Knee Osteoarthritis: The Multicenter Osteoarthritis Study.”3 The abstract was presented by coauthor Tuhina Neogi, MD, PhD, FRCPC, professor of medicine at Boston University, in place of lead author Jia Liu, MD, who was on maternity leave.
Researchers suspect that neural processing plays a role in the evolution of pain patterns for some knee OA patients, said Dr. Neogi. “Early on in the course of disease, response to initial injury is appropriate, because we know that nociceptors in the joint tissue are responding. But later, as pain becomes chronic and persistent, this no longer represents pure nociception. This raises the possibility that there are altered neurological pathways that may play a role in the transition of pain patterns in osteoarthritis.”
Both peripheral and central sensitization can increase sensitivity to stimuli, she said. “But whether sensitization has effects on the evolution of knee OA-related pain is unknown.”
‘About 15% of patients who undergo TKA have residual, moderate-to-severe joint pain that persists two to five years after the procedures.’—Dr. Singh
Data on 1,951 older adults with, or at high risk for, knee OA were used for the assessment. The mean age of participants was 68; 60% were female, and their mean body mass index was 31. Around 8% of the participants in the study developed constant pain over the two-year period. Pressure pain threshold (PPT), or the point at which participants first felt pressure change to slight pain, was measured at the wrist and patella using an algometer. Participants also completed the Intermittent and Constant OA Pain (ICOAP) questionnaire at baseline and two years later. Lower PPT scores indicate more pain sensitization. At the patella, the site of disease, it indicates peripheral and/or central sensitization, and at the wrist, it indicates central sensitization, said Dr. Neogi.
The study found that lower levels of peripheral and central pain sensitization were both associated with lower rates of progression from intermittent or no pain to constant pain.
“Sensitization appears to play a role in changing a patient’s pattern and the severity of OA-related pain,” said Dr. Neogi. “This has implications for understanding the transition from acute to chronic pain and may offer opportunities for targeted treatment.”
Imaging Techniques
Chaiwut Siriphithakwong/shutterstock.com
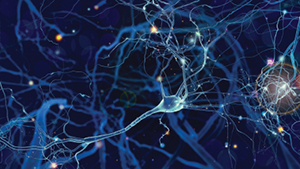
In a new study of central nervous system pain pathways in rheumatoid arthritis (RA), researchers assessed neural changes before and after disease-modifying therapy with pulsed arterial spin labeling, a type of functional magnetic resonance imaging (fMRI).
“Functional neuroimaging has enabled the identification of supraspinal networks that modulate pain and permits a more quantitative assessment of the pain experience,” said Yvonne C. Lee, MD, MMSc, assistant professor of medicine at Brigham and Women’s Hospital in Boston.4 Dr. Lee is also lead author of the abstract, “A Pilot Pulsed Arterial Spin Labeling Study of Regional Cerebral Blood Flow in Response to Pain in RA, Before and After DMARD Treatment.”5
The study began with a cross-sectional analysis of 15 patients with active RA disease compared with 16 age- and sex-matched controls, followed by a prospective analysis of 10 RA patients followed for 12 weeks after they started standard DMARD treatment, said Dr. Lee. Researchers performed six-minute, pulsed arterial spin labeling on all subjects to assess regional cerebral blood flow. Experimental pain stimulus was performed using a pressure cuff inflated to achieve pain scores of 40 out of 100 on the hands of RA patients. The same pressure was used for the matched controls.
RA patients found the pressure more painful than the controls. They also had significant, stimulus-induced increases in regional cerebral blood flow in the medial prefrontal cortex and anterior cingulate cortex, which the controls did not.
“However, after 12 weeks of DMARD treatment, regional cerebral blood flow in the hand pain condition decreased to levels similar to that of the controls,” in these two cortices, said Dr. Lee. These findings suggest that pulsed arterial spin labeling may be useful to identify central nervous system pathways involved in RA pain regulation.
Opioids’ Serious Risks
Controversy surrounds opioid use for chronic pain due to abuse and mortality risks. “It’s all over the news today. There’s an epidemic of opioid use and bad consequences in adults in the U.S.,” said Cecilia P. Chung, MD, MPH, a researcher at Vanderbilt University Medical Center in Nashville. Data from the Centers for Disease Control and Prevention showed high rates of opioid-related emergency department visits and overdose deaths in recent years.6
Do different opioids, including long-acting forms, vary in their mortality risks? A retrospective cohort study, “Comparative Safety of Long-Acting Opioids for Non-Cancer Pain,” compared the safety of three widely prescribed long-acting opioids: morphine slow-release (SR), oxycodone controlled-release (CR) and transdermal fentanyl.7 The study used data on 50,658 patients enrolled in Tennessee Medicaid, including individuals with cancer or other serious diagnoses. The primary outcome was out-of-hospital mortality.
Long-acting opioids were prescribed primarily for musculoskeletal pain in 90% of the cases studied, said Dr. Chung. Six hundred and eighty-nine deaths occurred during 44,385 person-years of follow-up. Although all-cause mortality did not significantly differ between patients taking transdermal fentanyl and morphine SR, “the risk for both out-of-hospital, all-cause mortality and opioid-related mortality was 21% lower in patients taking oxycodone SR compared with those taking morphine SR,” she said.
Analgesic Exercise?
Postmenopausal breast cancer patients on aromatase inhibitors (AIs) who experienced arthralgia, a common treatment side effect, found pain relief with exercise according to findings reported in “Pain and Sensitization in Women with Aromatase Inhibitor-Induced Arthralgia,” presented by lead author Monica Crespo-Bosque, MD, a resident at Boston University Medical Center.8
“About 70% of breast cancer is estrogen receptor-positive, and AIs decrease estrogen levels by inhibiting the conversion of androgen precursors to estrogen, both in the peripheral and breast tumor tissue,” said Dr. Crespo-Bosque. “About 50% of these patients will get arthralgia, and many of them won’t complete their indicated course of treatment because of it.” Arthralgia may be related to estrogen deprivation in these women, because estrogen is though to have anti-nociceptive effects, she added.
For the Hormones and Physical Exercise (HOPE) study, the researchers randomized 121 postmenopausal women with a history of breast cancer who had been treated with AIs for at least six months and had arthralgia to either an aerobic exercise intervention or usual care. The exercise regimen included supervised resistance training twice weekly and 150 minutes of weekly aerobic exercise. The researchers measured pain severity and location using self-reporting, and assessed pain sensitization by measuring PPT at the knee and wrist with a handheld algometer.
Patients in the exercise group showed improvements in their pain severity, but no significant change in their PPT at the knee or wrist, so pain improvement must occur through mechanisms other than decreased sensitization, said Dr. Crespo-Bosque. Because AI-associated arthralgia may be due to sensitization, this patient population could provide insights into how pain develops and exercise’s positive effects on sensitization.
Susan Bernstein is a freelance journalist based in Atlanta.
References
- Singh JA, Nobel L, Weissman N, et al. Post-arthroplasty pain trajectories after total knee arthroplasty and their association with 6- and 12-month pain (abstract). Arthritis Rheumatol. 2016;68(suppl 10).
- Singh JA, Gabriel S, Lewallen D. The impact of gender, age, and preoperative pain severity on pain after TKA. Clin Orthop Relat Res. 2008 Nov;(466)11: 2717–2723.
- Liu J, Frey-Law L, Hawker G, et al. Relation of pain sensitization to the evolution from intermittent to chronic, persistent pain in knee osteoarthritis: The multicenter osteoarthritis study (abstract). Arthritis Rheumatol. 2016;68(suppl 10).
- Coghill RC, McHaffie JG and Yen YF. Neural correlates of interindividual differences in the subjective experience of pain. Proc Natl Acad Sci USA. 2003 Jul 8;100(14):8538–8542.
- Lee YC, Fine A, Protsenko E, et al. A pilot pulsed arterial spin labeling study of regional cerebral blood flow in response to pain in RA, before and after DMARD treatment (abstract). Arthritis Rheumatol. 2016;68(suppl 10).
- Centers for Disease Control and Prevention. Vital signs: Overdoses of prescription opioid pain relievers and other drugs among women: United States, 1999–2010. MMWR Morb Mortal Wkly Rep. 2013 Jul 5;62(26):537–542.
- Chung CP, Dupont W, Murray K, et al. Comparative safety of long-acting opioids for non-cancer pain. Arthritis Rheumatol. 2016;68(suppl 10).
- Crespo-Bosque M, Brown C, Cartmel B, et al. Pain and sensitization in women with aromatase inhibitor-associated arthralgias. Arthritis Rheumatol. 2016;68(suppl 10).