Another critical component is the collection of all patient data in a common registry, the ACR Rheumatology Clinical Registry. According to Dr. DeWitt, data are analyzed in aggregate and at the individual site level to allow for benchmarking and sharing of best practices. “During these action-period calls that occur every month, we review the data and we look at where we are improving and where we need to improve,” she says.
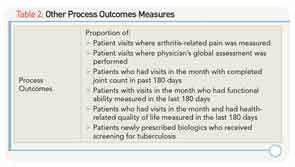
A current focus across the learning network teams is previsit planning. “Previsit planning is members of a care team preparing in advance of the patient visit to best meet [the patient’s] needs,” says Dr. DeWitt. “We can review performance on the process measures at the patient level (e.g., labs, uveitis screening) like a checklist, and during previsit planning, teams can review how patients are doing in terms of disease control and if treatment changes might be made.” This process may lead to more efficiency, standardization of care practices, and freeing up time during the visit to address priority areas to the patient, she added.
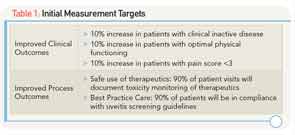
Aggregate data show that toxicity monitoring is above target at 92% for patients just prescribed disease-modifying antirheumatic drugs (DMARDs) and about 78% for patients who have been on DMARDs longer. Uveitis screening is about 88%, Dr. DeWitt says.
Reports from the Field: What Participants in PR-COIN Have to Say
For Stacy Ardoin, MD, assistant professor of rheumatology and immunology at Nationwide Children’s Hospital, Columbus, OH, participation in PR-COIN has resulted in a number of important improvements in JIA care. She says, for example, that she and her collegues have started collecting some standard outcome measures that they previously were not collecting, such as a regular pain score, by documenting the joint count in a consistent way, and assessing the general activity of disease. The monthly reports they get through PR-COIN show that they’ve made tremendous increases in all functional measures. “For example,” she says,” collecting a pain measure went from 0% to 100% and documented joint count went from 20% to 80%,” she says.
Ronald Laxer, MD, a rheumatologist at the Hospital for Sick Children in Toronto, Ontario, also says that his institution has seen significant improvement in a number of process measures since the launch of the initiative. For example, he says that although he and his colleagues thought they were monitoring their JIA patients to get their eyes checked at certain intervals, when they looked at their medical charts they found that only about 10% of patients had reports from their ophthalmologists. “So with the support of PR-COIN we instituted new processes and we are up to about 60% of patients who now have ophthalmology reports included in the medical records,” he says.