The Physician Quality Reporting Initiative (PRQI) is a voluntary quality reporting program initiated by the Centers for Medicare and Medicaid Services (CMS) in 2007. CMS provides bonus payments to eligible providers who successfully report on applicable PQRI measures. For 2010, rheumatologists who successfully participate in PQRI can earn an incentive payment of 2% of the total Medicare Physician Fee Schedule–allowed charges for services provided during the 2010 reporting period. Here are answers to some of the most common questions regarding PRQI.
Am I Eligible, and Where Do I Sign Up?
Most rheumatology providers who are paid under the Medicare fee schedule meet the ”Eligible Provider” definition and qualify to participate in PQRI, including nonphysician providers such as physician’s assistants and nurse practitioners. For a list of providers eligible to participate in the PQRI program, visit www.cms.gov/pqri. Registration with CMS is not required to participate in the PQRI program.
How Do I Get Started?
There are two mechanisms for submission, multiple reporting options, variances in measures to be reported, and a timeframe for reporting. To start, first choose your reporting mechanism, then what measures you will report on, and lastly, a timeframe to submit quality data.
Reporting Mechanism
Providers have the option of reporting PQRI measures through claims or through a qualified PQRI registry.
Claims Based
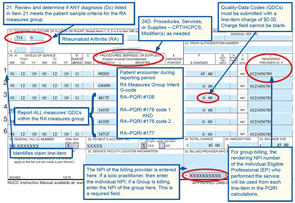
To report PQRI through claims submitted to CMS, the provider will add a CPT II code to an appropriate patient encounter/claim. An appropriate claim includes the CPT code, ICD-9 code, and any other codes included in the denominator of the PQRI measure. The CPT II code is a five-digit alphanumeric code used to report that an action has been taken, or not taken, to satisfy a measure.
As with CPT coding, there are modifiers to be used in conjunction with the CPT II codes for some of the PQRI measures. These modifier codes are intended to capture valid reasons why an action was not taken.
Remember, the PQRI bonus payments are based on participation, not performance; using the proper modifier codes will ensure that your reporting is accurate.
- 1P exclusion modifier due to medical reasons
- 2P exclusion modifier due to patient reasons
- 3P exclusion modifier due to system reasons
In addition, CPT II codes for PQRI reporting have a modifier to signify that the recommended action was not taken, without a valid reason documented:
- 8P reporting modifier—action not performed, reason not otherwise specified
Reporting the 8P modifier if the action was not taken is important to ensure successful PQRI reporting.
