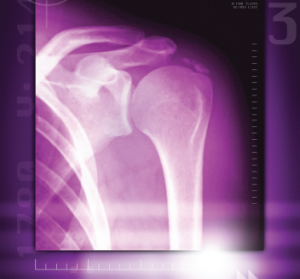
A colored X-ray of a calcified shoulder joint reveals a deposit of calcium at the top right of the shoulder joint.
Miriam Maslo / Science Source
MADRID—Calcification in osteoarthritis (OA) involves a series of pathways and interactions that feed off each other in a process that bears some resemblance to the transformation of cartilage to bone that takes place in the embryonic stage of human development, a researcher said here at the 2017 Annual European Congress on Rheumatology (EULAR).
“My hypothesis is that osteoarthritis is a restart of endochondral ossification in the adult organism,” said Jessica Bertrand, PhD, professor of orthopedic surgery at Otto-von Guericke University in Madgeburg, Germany. “The chondrocytes seem to differentiate into a more hypertrophic state, similar to endochondral bone formation.”
Dr. Bertrand’s research found this differentiation process is activated as the amount of calcification increases in vivo and in vitro. “This [finding] indicates a link between chondrocyte hypertrophy and cartilage calcification,” she said.
She described a key role of the pyrophosphate pathway, which is involved in the production of basic calcium phosphate (BCP) crystals.
In their OA cohort and in mouse models, increased expression of collagen X was linked with an increase in calcification, while greater expression of nucleotide pyrophosphatase phosphodiesterase (NPP1) was associated with decreased calcification.1 Then, through BCP interaction with the extracellular matrix, the LRP6 receptor is phosphorylated in the canonical Wnt pathway, which has been implicated in bone disease, leading to the differentiation of chondrocytes. Dr. Bertrand called it “a vicious cycle.”
“BCP crystals perpetuate the hypertrophic differentiation of chondrocytes,” she said. “The data suggest that OA is characterized by the reactivation of molecular signaling cascades that, at least in part, resemble endochondral ossification.”
Calcific Tendinopathy
Christelle Darrieutort-Laffite, a PhD student in rheumatology at the University of Nantes in France, said a new analysis of cadaver samples produced somewhat surprising findings on calcific tendinopathy in the rotator cuff that shed light on the nature of the disease, but also raise other questions. This is a common disease, Dr. Darrieutort-Laffite said, but its origin is still mostly unexplained, with the molecular and cellular mechanisms not well identified.2
In the study, researchers collected samples from cadavers and used ultrasound to find calcified tendons. Then they were analyzed with micro computed tomography (CT) to assess how the deposits were distributed. Several types of histological staining were performed.
Researchers found several patterns. In two samples, small calcifications were spread between fibers in the tendons. In two others, larger deposits were encapsulated in fibrous tissue. In another, osseous changes to the tissue were seen in the tendon.
In the peripheral areas of the larger calcifications, researchers found that the cells were similar to chondrocytes, because they expressed the transcription factors Runx2 and Sox9, which are associated with cartilage formation. But they found the cells in this area did not express collagen II, a critical protein found in articular cartilage.
Calcification in the cartilage can be associated with the death of chondrocytes, so investigators looked for caspace-3, a protein that’s linked with apoptosis of these cells. But they found that those chondrocyte-like cells around the larger calcifications actually didn’t express this protein.
Dr. Darrieutort-Laffite said the findings likely indicate the various stages of the disease. “Chondrocyte-like cells were observed around larger deposits and could be involved in the mineralization process,” researchers wrote. “Interestingly, they differ from the cells of the fibrocartilage as they did not express collagen II.”
Dr. Darrieutort-Laffite said more investigation needs to be done to understand the mechanisms at work. “Further analyses are necessary to understand the first steps of the process and the regulatory factors involved,” she noted.
Imaging
Another study by French researchers found that ultrasound of the wrist performed better than traditional X-ray in detecting calcium pyrophosphate deposition (CPPD), said Alice Combier, MD, a rheumatology resident at the Bichat Hospital in Paris.3
In the study, 32 patients with CPPD and 26 controls, who had other rheumatic diseases, including rheumatoid arthritis and spondyloarthritis, had a wrist ultrasound performed and X-rays taken of the wrist. Blinded reviewers looked for what researchers called chondrocalcinosis (CC)—imaging features that suggest CPPD.
CC was found on ultrasound in 30 joints and on X-ray in 17 joints in the CPPD patients, amounting to a significant difference (P<0.001). The sensitivity and specificity of ultrasound were 94% and 85%, respectively, compared with 53% and 100% for radiography.
Researchers also found that on ultrasound, sensitivity was higher, at 81%, at the triangular fibrocartilage, than at the radiocarpal joint, at 50%.
“Our study suggests,” Dr. Combier said, “that wrist ultrasound should be considered a relevant tool for the diagnosis of CPPD, with higher sensitivity than radiography.”
Thomas R. Collins is a freelance writer living in South Florida.
References
- Bertrand J, Nitschke Y, Fuerst M, et al. Decreased levels of nucleotide pyrophosphatase phosphodiesterase 1 are associated with cartilage calcification in osteoarthritis and trigger osteoarthritic changes in mice. Ann Rheum Dis. 2012 Jul;71(7):1249–1253. doi: 10.1136/annrheumdis-2011-200892. Epub 2012 Apr 17.
- Darrieutort-Laffite C, Najm A, Garraud T, et al. Histological characterization of rotator cuff calcific tendinopathy (abstract OP0190). Annual European Congress of Rheumatology. 2017 Jun 15. Madrid, Spain.
- Combier A, Forien M, Gardette A, et al. Comparison of ultrasonography and radiography of the wrist for diagnosis of calcium pyrophosphate deposition (abstract OP0191). Annual European Congress of Rheumatology. 2017 Jun 15. Madrid, Spain.
