The ICD-10 page on the Centers for Medicare & Medicaid Services (CMS) website features a countdown clock that shows the time left until Oct. 1, 2015, the date on which compliance with the new code set becomes mandatory. By the time this issue goes to press, the clock will read 90 or fewer days.
Time feels as though it has been perpetually counting down to ICD-10—the International Classification of Diseases, Tenth Revision—but the clock is actually running out now. After the initial decision to switch in 2009 and two yearlong delays, Oct. 1, 2015, now marks the official go-live date for the significantly revised and expanded coding language.
As with any major process change, ICD-10 comes with both benefits and challenges. On the plus side, ICD-10 carries the potential for increased international collaboration, the collection of more detailed health data and more precise documentation of the patient experience. Ultimately, this should lead to better analysis of disease and its progression, facilitate better quality of care and improve treatment outcomes. It’s also expected to contribute to epidemiological research and population health management.

Dr. King
“We’ll get a lot more granular data about what’s happening to our patients … such as a fracture from a car accident when the patient wasn’t wearing a seatbelt,” says Charles King II, MD, North Mississippi Health Services, Tupelo, Miss., and an ACR Board Member. “We’ll get information about quality, so third-party payers are going to use the data with these specific codes to figure out if they’re paying claims correctly. It’ll allow more robust data collection. We’re going to understand the causality of diseases and injuries to a much more in-depth degree.”
On the flip side, the challenges inherent with the switch include the significantly increased scope, technical difficulties, training needs and financial risks, and these issues are projected to be unevenly experienced by physicians who work in hospital systems, multispecialty groups and smaller private practices. Despite the varying level of complications, one truth is clear—the switch is not optional, and the time is now to make sure everything’s in place when the clock runs out in October.
The Timeline So Far
ICD-10 codes must be used on all HIPAA transactions, including both outpatient claims with dates of service and inpatient claims with dates of discharge of Oct. 1, 2015, and beyond. The penalty for submitting claims and other transactions with outdated codes is that they may be rejected and need to be resubmitted, which could result in delays and affect reimbursements.
According to CMS, the transition to ICD-10 is occurring because ICD-9 produces limited data about patients’ medical conditions and hospital inpatient procedures; the data set is 30 years old, has outdated terms and is inconsistent with current medical practice; and the structure of ICD-9 limits the number of new codes that can be created. In being more specific, ICD-10 contains significantly more codes than the previous iteration of the data set, and the codes are longer.
In ICD-9, there are about 14,000 diagnosis codes and 3,800 procedure codes, totaling about 17,800. By comparison, ICD-10 has nearly 70,000 diagnosis codes and nearly 72,000 procedure codes, for a total of almost 142,000 codes.
In addition to the increased quantity of codes, the new code structure poses challenges. Although there are some similarities (e.g., the hierarchal structure, the meanings of the symbols and the criteria for code assignment of the principal diagnosis code), some differences will take getting used to. The most significant difference is the code structure: where ICD-9 codes contain three to five characters, ICD-10 codes contain up to seven alphanumeric characters. Further, the “V” and “E” codes from ICD-9 are being discontinued, and the sixth digit in ICD-10 will mainly be numeric, and identify laterality and drug poisoning.
“[The ICD-10] codes have a different structure, so there are different letters and numbers involved,” says Will Harvey, MD, MSc, Tufts Medical Center, Boston, chair of the ACR Government Affairs Committee. “It’s not inherently intuitive to anyone who just looks at the list, and there’s a great deal more specificity.”
The most significant difference [between ICD-9 & ICD-10] is the code structure: Whereas ICD-9 codes contain three to five characters, ICD-10 codes contain up to seven alphanumeric characters. Further, the ‘V’ and ‘E’ codes from ICD-9 are being discontinued, & the sixth digit in ICD-10 will mainly be numeric, & identify laterality & drug poisoning
Take a fracture for example, Dr. Harvey explains. Although ICD-9 has a single code for a fracture, ICD-10 has much more specificity, and the code integrates numerous details, such as right or left arm, compound fracture or not, healed or not healing, as well as other complications. “Another example specific to rheumatology is that [the] number of codes for rheumatoid arthritis goes from 10 to 246,” he adds. “It will take time for people to get a grasp [on] how to use the specific nature of these new codes.”
Learning the new code structure will be a big transition, Dr. King says. “Some of the nomenclature that goes with the codes is not what we’re used to, and it’s not as intuitive as ICD-9. … For some diseases, instead of one code, there may be many codes to explain a single disease. There’s not always a one-to-one code conversion; it can be one to many or one to one, and that’s certainly challenging.”
The ACR has taken numerous actions to try to mitigate the burden of ICD-10 implementation on physicians, including offering training programs and workshops at various meetings nationwide, publishing online resources and information, and promoting legislation to protect physicians. In the legislative arena, the ACR signed a resolution passed at the American Medical Association’s November 2014 meeting to skip the implementation of ICD-10 and move directly to ICD-11, which is slated to begin beta testing in 2015.

Dr. Harvey
Additional legislative work has continued, and ACR representatives spent all winter 2014–2015 working on proposed legislation. As a result, H.R. 2240 was introduced by Rep. Black (R-TN) in May. Dr. Harvey says the legislation has two components. First, it “requires CMS to offer end-to-end testing for anyone who wants [it] and [certify] to Congress that the system performs as well as the current one in terms of rate of denied claims; and next, [it establishes] a safe harbor period that prevents rejection of claims based on inaccurate subcode detail.”
The safe harbor period has been part of legislative efforts for over a year now. On Feb. 12, 2014, the AMA sent a letter to then Secretary of Health and Human Services Kathleen Sebelius, urging the CMS to reconsider ICD-10 implementation. One point was to encourage CMS to adopt a policy for Medicare that provides an “implementation” period during which payment cannot be denied on the basis of the ICD-10 code specificity.
“We’re hoping there will be some period of time—ideally 18 months—where you use the ICD-10 code and you have to get the main part of the code right, but this specificity part we can get a pass for a period of time where we’re not held responsible for honest mistakes related to that,” Dr. Harvey explains.
Editor’s note: Since this article was written, the CMS has acted on the requests of the ACR and others and announced a one-year grace period during which it will not deny claims on the basis of incorrect ICD-10 sub-codes, so long as the correct family of codes is used. It also made some other concessions. See the related news.
Technical Difficulties
With the significant changes between the code sets, how CMS plans to test the system in advance has been a key topic of conversation in the medical community and on Capitol Hill. Getting the initial testing week, held March 3–7, 2014, on the calendar was a positive outcome for the ACR and other professional organizations that had been lobbying for testing. However, this first pass did not represent true end-to-end testing because it only tested the CMS system, as opposed to going from the provider through any intermediaries to CMS, being processed and then going back to the provider.
In response to an outcry from the medical community, CMS announced that there would be three end-to-end testing periods in 2015 involving a total of 2,550 volunteers. The testing periods include the submission of test claims to Medicare and then a subsequent response, called a remittance advice (RA), which explains the adjudication of the claims. With the testing period, CMS intends to demonstrate that providers can successfully submit claims through Medicare, that software changes made at CMS to support ICD-10 result in appropriately adjudicated claims (based on the pricing data used for testing purposes) and that accurate RA documents are produced.
To facilitate the testing, CMS required Medicare administrative contractors (MACs) to conduct limited end-to-end testing with submitters. Test claim submissions were scheduled for Jan. 26–30, April 27–May 1 and July 20–24, 2015. The expectation was that testers would be selected randomly to “represent a broad cross-section of provider types, claims types, and submitter types,” including between five and 15 clearinghouses, as noted in the CMS MLN Matters No. SE1409 (Rev. Dec. 8, 2014).
Although this expansion of the testing initiative is an improvement, it’s not exactly what the ACR was hoping for, Dr. Harvey says. The current claim acceptance rate is 97% for ICD-9 codes, he explains, and the first tests held in January resulted in approximately 80% acceptance, and only 3% were rejected because of ICD-10 code problems. “We believe that everyone who wants to should have the opportunity to test,” he says, “but this is still a huge step from where they were a year ago. … I remain particularly concerned for the thousands of solo or small group practices [that] will have to rely on believing they are similar enough to other practices [that] actually got the opportunity to test, because the vast majority of them will not be one of the 2,550.”
Another aspect of the technical challenge is that Oct. 1, 2015, happens to be a Thursday—which means that claims submitted on Wednesday that week will need to be handled differently on Thursday. Further, there will be a period of time in which claims need to be processed in both formats, depending on dates of service. Billing professionals will have to be extra vigilant and watch service dates for a while to ensure that claims are processed correctly.
Learning the New Code
One especially important aspect to being prepared for the go-live is to provide staff training ahead of time. Staff training will be key for ensuring a smooth transition to the new coding set and for keeping the day-to-day practice of documenting and billing on track.
To help ensure that staff members are successful after ICD-10 goes live and that there are minimal disruptions to practice, the ACR recommends categorizing which staff members need to receive training and at what levels, coordinating the timeline for training and working with the team on completion, identifying the training format that works best for the team (e.g., classroom, online, conference), deciding on the amount of downtime for the office during training and identifying what additional resources staff members will need after training is completed.
In particular, the ACR identified three groups and levels that are integral to ensuring proper staff training:
- Administrative staff (e.g., schedulers, receptionist)—overview and general understanding of the new ICD-10 code structure;
- Clinical staff (e.g., physician assistants, nurses, nurse practitioners)—clinical concepts and level of detail in ICD-10 for documentation purposes; and
- Physicians and coders—clear understanding of the new code structure, coding guidelines and conventions related to specificity.
In addition to receiving in-depth training on ICD-10, coders who hold a coding membership from the AAPC will need to complete a proficiency assessment by Dec. 31, 2015, to satisfy their certification maintenance requirement.
In many cases, physicians are relying on their EMR vendor for training or to ensure a smooth transition. Elena Weinstein, MD, of Arthritis and Rheumatology of Denver, is contracted with an EMR/billing provider, “and the program does much of the work for ICD-10. We have no paper charts, and all our billing is electronic, so no superbills,” she says.
Another consideration during training periods is how to collaborate when numerous people need to enter data into the EMR. This challenge is known as “chart etiquette,” Dr. King explains. “Providers will need to keep problem lists current, removing old or inactive problems promptly. You can imagine how large a problem list can be if 15 different specialties all enter problems specific to their field. It potentially reaches the point of being unmanageable. Healthcare systems need to start thinking about how to manage both problem and medication lists correctly in the medical record.”
There will be a period of time in which claims need to be processed in both formats, depending on dates of service. Billing professionals will have to be extra vigilant & watch service dates for a while to ensure that claims are processed correctly.
Budgeting & Financial Considerations
Staff training time and resources are important, although this constitutes a financial consideration in the transition. Training time, software upgrades and other considerations are all rolled into current projections on the cost of implementing ICD-10 across the U.S. And the total cost is projected to be significant.
The Nachimson Advisors released a revision to the 2008 study on the costs of ICD-10 implementation that projects higher costs than originally estimated for practices of all sizes. The practice definitions were small practice (i.e., three physicians and two administrative staff), medium (i.e., 10 physicians, one full-time coder and six administrative staff) and large (i.e., 100 physicians, 64 coding staff, 10 full-time coders and 54 medical records staff). The updated projections from 2008–2014 include the following:
- Small practice: $83,290 vs. $56,639–226,105;
- Medium practice: $285,195 vs. $213,364–824,735; and
- Large practice: $2,728,780 vs. $2,017,151–8,018,364.
The revised projections are the results of adding in tasks that were not considered “critical” in the 2008 study, which includes testing, as well as projections for payment disruptions.
There is a general expectation that there will be an increase in denied claims and delays in reimbursements as the country gets used to ICD-10. AMA predicts, “You will have disruptions in your transactions being processed and receipt of your payments. Physicians are urged to set up a line of credit to mitigate any cash flow interruptions that may occur.” Planning ahead and having cash reserves on hand to keep business moving while these difficulties are sorted out could make the difference.
Getting Ready
Although the AMA continues to seek a repeal of ICD-10, the overall sentiment is that ICD-10 is coming, and the clock is running out. Many hospital systems, multispecialty groups and physicians’ offices have begun implementation efforts and training for their staff. Those that have not are encouraged to get started quickly.
“It’s still not too late, but we’re almost past the point where if you haven’t started dipping your toe in the water, you’re going to have to jump in all the way,” Dr. King says. “Start working with your vendor to make sure your system is capable of converting to ICD-10. Start participating in webinars or attending educational sessions, for example, the ACR program, to start learning. If dual coding is possible, start doing that now and prepare, so most of your codes are already in place by the time ICD-10 goes live.”
The AMA recommends several steps that need to be taken to prepare for converting to ICD-10:
- Talk to your practice management or software vendor about whether the needed software updates will be installed with upgrades and when;
- Talk to your clearinghouses, billing service and payers to determine when they will have their ICD-10 upgrades completed and when you can begin testing with them;
- Identify the changes that you need to make in your practice to convert to the ICD-10 code set (e.g., diagnosis coding tools, superbills, public health reporting tools);
- Identify staff training needs, and complete the necessary training;
- Conduct testing internally to ensure transactions with ICD-10 codes can be generated; and
- Conduct testing externally with clearinghouses and payers to ensure transactions with ICD-10 codes can be sent and received.
Patient Impact
After the steps have been taken to lay the groundwork for the go-live, another consideration is what to communicate with patients. The code switch will take some getting used to for healthcare providers across the country, so that carries with it the risk that the physician will lose overall productivity.
“Does it impact patients? It absolutely does,” Dr. King says. “It’s one more step toward losing some of the feel of the patient–physician relationship. When we go live, physicians will have to spend much more time coding with their eyes on the computer instead of spending time observing the patient.”
In Dr. Weinstein’s case, “We haven’t told our patients anything,” she says, “although as it gets closer, we may just ask for a little extra patience.”
Ultimately, the way things look as of mid-May 2015, the switch is coming without further delay, and the changeover has the potential to cause some considerable upheaval for day-to-day medical practice. The only way to mitigate that is to be prepared.
“The message is get ready. Now,” Dr. Harvey says. “Leverage every resource you can afford and start preparing.”
Kimberly J. Retzlaff is a medical journalist based in Denver.
Resources to Help You Gear up for ICD-10
Numerous resources, both online and in person, are available to help physicians and their staff switch to the ICD-10 code set.
- Attend a coding course (specialty or broader)
- The ACR’s online resources
- The ACR Practice Management Department: 404-633-3777; [email protected]
- Road to 10: The Small Physician Practice’s Route to ICD-10. CMS.
- Talking to your vendors about ICD-10: Tips for medical practices. CMS.
- Ullman K. Plan now for the ICD-10 changeover. The Rheumatologist, May 2011.
- Buckholtz R. So you were a procrastinator … now how do you prepare for ICD-10? AACP.
Case Studies of ICD-9 vs. ICD-10 Coding
Coding examples provided by Trina Gee, RHIT, coding supervisor, Northwest Medical Center, Tucson, Ariz. These codes are based on the ICD-10 coding logic that was current as of May 19, 2015, and is subject to change with the final coding changes effective Oct. 1, 2015.
ICD-10 Timeline
2009 ICD-10 announced and go-live slated for October 2013
Aug. 27, 2012 HHS announced a one-year delay of ICD-10 implementation, pushing the date to Oct. 1, 2014
Feb. 19, 2014 The federal government agreed to conduct end-to-end testing on ICD-10 for select providers
March 3–7, 2014 Testing week
Apr. 1, 2014 Go-live delayed to October 2015 via the Protecting Access to Medicare Act of 2014 (Pub. L. No. 113-93)
Jan. 26–30, 2015 CMS conducted the first of three rounds of end-to-end testing
April 27–May 1, 2015 CMS conducted the seond of three rounds of end-to-end testing
July 20–24, 2015 CMS scheduled the third of three rounds of end-to-end testing
Oct. 1, 2015 Go-live
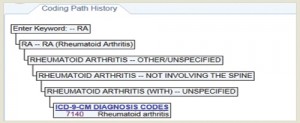
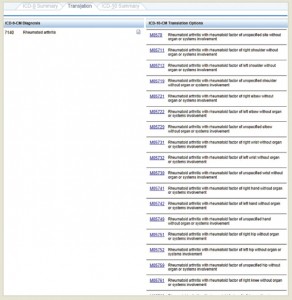
(Click for larger image) Example 1.a.1: Rheumatoid Arthritis (RA)—The coding path shows the decisions made by the coding specialist to obtain the ICD-9 diagnosis code for RA.
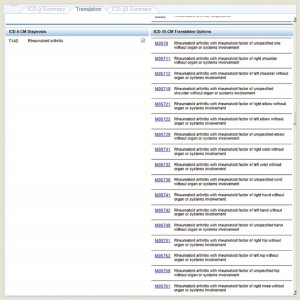
(Click for larger image) Example 1.a.2: RA—The Translation tab demonstrates the numerous possible ICD-10 codes (right) that correspond to the single ICD-9 code for RA.
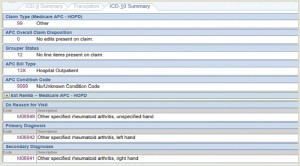
(Click for larger image) Example 1.a.3: RA—The ICD-10 summary tab demonstrates the final selections and shows the ICD-10 codes for the Reason for Visit, Primary Diagnosis, and Secondary Diagnoses.
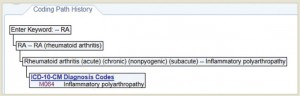
(Click for larger image) Example 1.b.1: RA with Polyarthropathy—The coding path shows the decisions made to obtain the ICD-10 diagnosis code for inflammatory polyarthropathy.
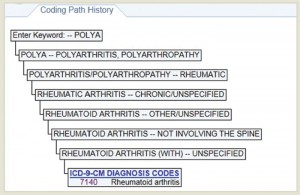
(Click for larger image) Example 1.b.2: RA with Polyarthropathy—The coding path shows the decisions made to obtain the ICD-9 diagnosis code for inflammatory polyarthropathy, which is the same as the code for RA without polyarthropathy.
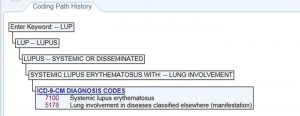
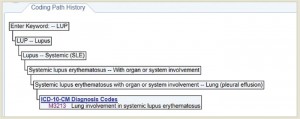
(Click for larger image) Example 2.a.1: Lupus—The coding path history shows the decisions made to obtain the ICD-9 diagnosis codes for lupus.

(Click for larger image) Example 2.a.2: Lupus—The Translation tab demonstrates the ICD-10 diagnosis code (right) that corresponds to the ICD-9 codes for lupus with lung involvement.
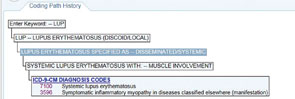
(Click for larger image) Example 2.b.1: Lupus—The coding path shows the decisions made to obtain the ICD-9 diagnosis codes for lupus with muscle involvement.
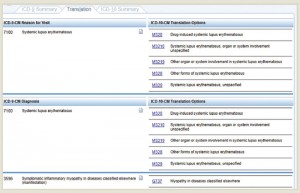
(Click for larger image) Example 2.b.2 Lupus—The Translation tab demonstrates the ICD-10 codes for the reason for visit (top right) and diagnosis (bottom right) that correspond to the ICD-9 codes for systemic lupus erythematosus.
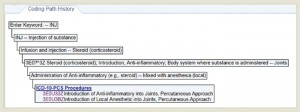
(Click for larger image) Example 3.1: Joint Injection—The coding path shows the decisions made to obtain the ICD-10 procedure code for a joint injection.
(Click for larger image) Example 3.2: Joint Injection—The Translation tab demonstrates the numerous possible ICD-10 diagnosis codes (right) that correspond to the single ICD-9 code for RA.
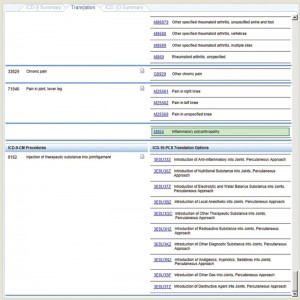
(Click for larger image) Example 3.2 continued: Joint Injection—The Translation tab demonstrates the numerous ICD-10 diagnosis codes (top right) that correspond to the ICD-9 codes for RA, chronic pain and pain in the joint, lower leg. The tab also demonstrates the possible ICD-10 procedure codes (bottom right) that correspond to the ICD-9 code for injection of therapeutic substance into joint/ligament.