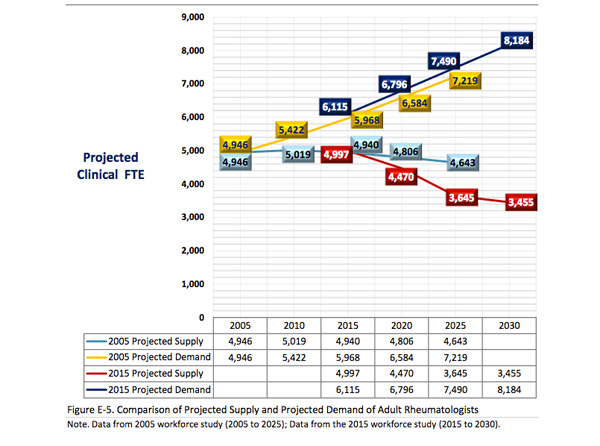
 In 2015, the U.S. hit a turning point in which the demand for rheumatologists outpaced the supply of physicians. For many, this demand, which is on pace to increase 27% by 2020 and 45% by 2025, requires creative recruitment strategies to attract physicians to private practice.1
In 2015, the U.S. hit a turning point in which the demand for rheumatologists outpaced the supply of physicians. For many, this demand, which is on pace to increase 27% by 2020 and 45% by 2025, requires creative recruitment strategies to attract physicians to private practice.1
What’s Working?
Research suggests large, urban practices on the East and West coasts are more attractive to physicians, a trend witnessed by Herbert Baraf, MD, FACP, MACR, senior member and managing partner of Arthritis and Rheumatism Associates with offices in Washington, D.C., and Maryland.
“Our practice hasn’t had terrible challenges finding people, but we know there is a limited number of applicants,” Dr. Baraf says.
An estimated 200–240 rheumatology fellows graduate and seek positions each year. Many newly minted rheumatologists choose research or academic positions. More than half of individuals completing their fellowship are international medical graduates, many of whom return to their home countries. Others look for employment at hospitals, health systems or other institutional entities. Such numbers may leave only 50–70 new rheumatologists interested in private practice nationwide, he explains. Ultimately, the pool of applicants looking for private practice positions is relatively small.
With 13 of the 20 physicians in his practice hired within the last 12 years, Dr. Baraf and his team have interviewed physicians who have come to the practice from different avenues. These avenues include:
- Word of mouth;
- Advertising using the ACR’s CareerConnection service;
- Engagement with trainees at lectures on finding a private practice;
- Attending fellows-in-training (FIT) programs at scientific meetings; and
- Direct contact with fellowship program directors.
“The challenge is the numbers game,” he says. “A practice looking to hire needs to provide an attractive opportunity to be successful.”
What Do Prospective Physicians Want?
Ethan Craig, MD, MHS, a third-year fellow at Johns Hopkins Hospital, Baltimore, believes the right offer depends on the person and their goals. He says, for many, the choice of practice will be dictated heavily by location and family considerations, and then by tangibles, such as compensation, practice setting and the details of the position.
Opportunities for career advancement and whether or not the position matches a physician’s goals will also be key factors for new graduates, Dr. Craig says.
“For an academically inclined person, this [interest] likely means finding a place that will provide protected time and resources for research, as well as an established program that meshes with their interests,” he says. “For others, it may be about the size of the group, the availability of options for partnership or advancement within an organization [for hospital affiliated practices], or opportunities/freedom to build a program.”
Dr. Craig says available support staff resources, including nurses and administrative help, at a practice are also attractive draws.
Make It Work
For practices restricted by geographic location, staff support and community amenities, strategies for recruitment are combined with creative approaches to ensure patient access to care.
Suzanne Gharib, MD, a rheumatologist in private practice in Charleston, W.Va., admits the odds of recruiting new physicians to private practice in her region are unfavorable. “Many hospitals in our area compete to recruit physicians. And even the university, [which] can offer positions with lucrative compensation packages, is having difficulty with recruitment.”
With only 15 practicing rheumatologists in the state, patient demand in W.Va. is outpacing the physician supply. This fact means Dr. Gharib and her colleagues work longer hours to see more patients. And each patient requires extra time to complete administrative work to manage insurance requirements, such as securing authorization for medication coverage. Given the rural setting of the state, many of these patients also travel two to three hours one way to visit a clinic, which complicates scheduling.
Two strategies are helping Dr. Gharib’s practice meet patient demands:
- Employing more mid-level support: By providing extra training to nurse practitioners and physician assistants, these mid-level staff members can see patients independently. Dr. Gharib and her practice colleagues are considering hiring a mid-level staff support person to fill the space currently open for an additional physician; and
- Coordinating with primary care physicians: After a recent meeting with a large primary care group in her area, Dr. Gharib and her colleagues are contemplating how primary care can provide a higher level of support to patients with low-acuity rheumatic conditions who can be managed in primary care.
“For us, a shortage of physicians means we must work together to establish plans for care that meet the needs of all patients, including those patients with severe disease, to ensure workforce issues don’t negatively [affect] patient wellbeing,” Dr. Gharib says.
Carina Stanton is a freelance science writer in Denver.
Reference
- ACR Committee on Training and Workforce Issues. 2015 workforce study of rheumatology specialists in the United States. ACR. 2015.
Resource
Learn more about rheumatology workforce research and discussion.