Discussion
The eye is frequently involved in SLE, with the most common manifestation being keratoconjunctivitis sicca. Other less common causes include cotton wool exudates due to retinal vasculitis, episcleritis and scleritis.
Rarely, the orbit can be affected.1 Orbital disease in patients with rheumatic disease may include primary inflammation of the orbital tissue (e.g., orbital pseudotumor or orbital inflammatory syndrome), inflammation of the extraocular muscles (e.g., orbital myositis), cavernous sinus thrombosis, retrobulbar hematoma, orbital cellulitis, Graves disease or contiguous spread of inflammation from the sinuses, which most typically occurs in ANCA-associated granulomatous vasculitis.2
The most common sign of orbital disease is proptosis caused by a space-occupying lesion or inflammatory process. Associated symptoms and signs include pain, blurred vision, diplopia (double vision) as a result of limitation of eye movement, eyelid swelling and displacement of the globe.3
Orbital pseudotumor, part of the spectrum of idiopathic orbital inflammation, is a nongranulomatous inflammatory disorder that may affect any structure in the orbit. It’s defined according to the orbital structures affected, with the presenting symptoms reflecting the degree of inflammation and the location of the inflamed tissue.4
There are several other reports of SLE presenting with proptosis due to orbital pseudotumor have been published.1,5,6
Patients with an acute presentation may complain of generalized malaise, in addition to ocular symptoms, but are generally afebrile; infections, such as orbital cellulitis, can mimic the features of orbital pseudotumor and should be excluded in patients with pyrexia.5
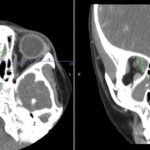
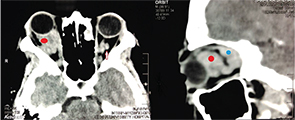
The diagnosis can be confirmed using CT or magnetic resonance imaging (MRI). In some cases, CT is preferred because of the inherent contrast by different attenuation values of the orbital fat, muscle, bony structures and air in the adjacent paranasal sinuses. Extraorbital extension is better delineated on MRI.
Systemic corticosteroids and immunosuppressive therapy aim to control the underlying disease and can decrease proptosis, improve visual acuity and ocular mobility, and reduce the associated symptoms. Rarely, orbital decompression may be necessary if the inflammatory process has caused proptosis severe enough to compromise the optic nerve (orbital apex syndrome).2