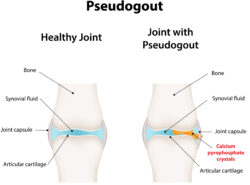
PHILADELPHIA—The term pseudogout has been a source of confusion among rheumatologists, especially as our understanding of calcium pyrophosphate crystal deposition (CPPD) disease has become more nuanced. This condition has many complex and interesting facets that warrant closer investigation.
An ACR Convergence 2022 session sought to update the audience on the progress to date in developing classification criteria for CPPD disease. The first speaker was Sara Tedeschi, MD, MPH, assistant professor of medicine at Harvard Medical School and Brigham and Women’s Hospital, Boston. She discussed the methodology and item considerations in developing the new classification criteria.1
Dr. Tedeschi noted that CPPD disease is common, but research on the condition has been stymied by the lack of validated classification criteria, reliance on synovial fluid polarized light microscopy for diagnosis and the disease’s diversity of presentations. These presentations can include acute CPP crystal arthritis (i.e., the condition historically called pseudogout), chronic CPP crystal inflammatory arthritis, osteoarthritis with CPPD and crowned dens syndromes.
Developing Classification Criteria
Using a four-phase process that began in 2019, the group working on the classification criteria used data and expert opinion from rheumatologists, a musculoskeletal radiologist and a methodologist from across the country and world to advance the project.
The first phase of the process was item generation, which included a literature review and the solicitation of suggestions from patients and a combined expert committee. The second phase was item reduction and refinement, which included discussions with an advisory group focused on clinical, laboratory and imaging data, as well as an item rating exercise by combined expert committee members. Here, Dr. Tedeschi referenced a paper she wrote with colleagues in which imaging features characteristic of CPPD on radiographs, computed tomography (CT) scans and dual-energy CT (DECT) studies were defined and a set of example images was compiled.2
In the study’s third phase, item weighting and threshold scoring was pursued. The group assembled a derivation cohort, which refers to a group of patients who would be used for testing some of the features of the classification criteria framework. Rheumatologists from 13 sites and six countries provided data from de-identified patients and were asked to rate their clinical suspicion for CPPD disease on a scale of -3 (least likely) to +3 (most likely).
Next, two blinded expert adjudicators from different institutions reviewed each case. The group then used data from the adjudicators, the rheumatologists who submitted the cases and information from synovial fluid analysis (when present) to define three patient categories: definite cases, definite mimickers (who then served as the control group) and uncertain. The group identified features of clinical cases that increased the odds ratio (OR) of a patient’s likelihood of having CPPD disease, such as if the patient ever had an acute inflammatory arthritis of the knee (OR 3.0, 95%; confidence interval [CI] 1.9–4.8) or the patient having more than one typical episode of acute inflammatory arthritis (OR 4.1, 95%; CI 2.5–6.7).