Background/Purpose
Psoriasis and psoriatic arthritis (PsA) are closely linked inflammatory conditions that can affect both children and adults. In children, these diseases are associated with traditional cardiovascular disease risk factors and subclinical atherosclerosis. In older adults, systemic inflammation from psoriasis and PsA accelerates atherosclerosis, and these conditions are independent risk factors for severe cardiovascular disease events including acute coronary syndrome, stroke, and cardiovascular death. While subclinical and accelerated atherosclerosis from systemic inflammation has been demonstrated, there have been no studies assessing the burden of non-fatal severe cardiovascular disease events in transition-age young adults with psoriasis and PsA.
Methods
We used data from the National Inpatient Sample database between 2016 and 2019, which comprises a stratified sample of patients admitted to hospitals in the U.S. Across all four years, they identified 1,406,913 records for patients aged 18–24. The researchers performed a cluster analysis to identify groups of patients with similar baseline health status based on comorbidities and personal demographics. The researchers then compared rates of admission for non-fatal cardiovascular disease events between patients with and without psoriasis, stratified by these clusters, to test the hypothesis that inflammation-driven atherosclerosis from psoriasis and PsA causes early cardiovascular disease events, and thus a higher rate of cardiovascular disease admissions, independent of baseline health and other comorbidities as indicated by cluster identity. This approach allowed the researchers to test this hypothesis empirically.
Results
Cluster analysis identified three distinct demographic groups as follows: Group 1) urban-dwelling higher-income patients of non-White or Black race/ethnicity with type 2 diabetes mellitus and obesity; Group 2) patients of white or Black race/ethnicity with type 1 diabetes mellitus, hypertension and hyperlipidemia; and Group 3) patients of white or Black race/ethnicity without a significant burden of traditional cardiovascular disease risk factors. In all three groups, transition-age patients with psoriasis or PsA were more likely to be admitted for a non-fatal cardiovascular disease event including heart failure, stroke, and acute coronary syndrome (Group 1 OR 1.72, P<0.0001; Group 2 OR 3.17, P<0.0001; Group 3 OR 1.20, P=0.0033). Group 2 had both a higher prevalence of psoriasis/PsA and a greater magnitude of difference in admission rates between patients with and without psoriasis/PsA compared to Groups 1 and 3.
Conclusion
These data are consistent with the researchers’ hypothesis that accelerated atherosclerosis from systemic inflammation in PsO and PsA leading to early cardiovascular disease events is a relevant concern for transition-age young adults beyond what can be explained by baseline health status and traditional cardiovascular disease risk factors. Further research is needed to develop cardiovascular disease prevention, screening, and risk stratification strategies for patients in this high-risk age group.
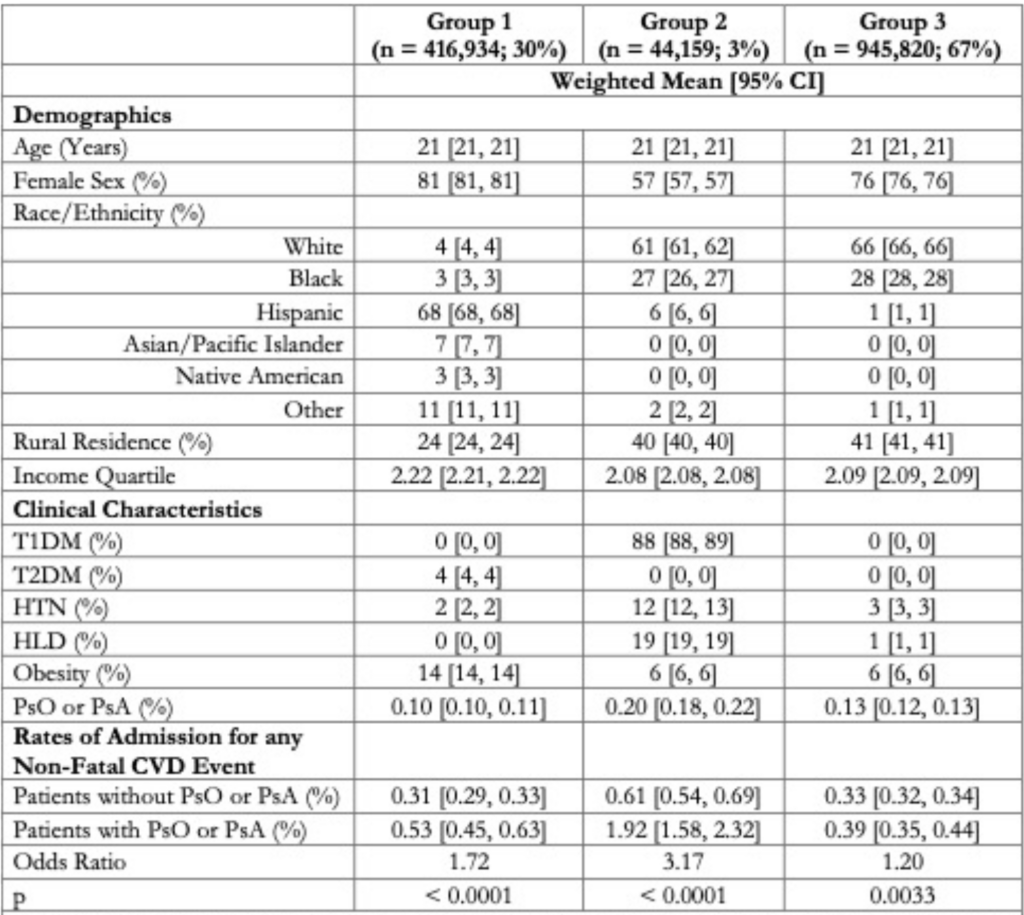
Table 1: Demographics, clinical characteristics and rates of non-fatal CVD admission for patients in Groups 1-3. Patients in Group 1 were significantly more likely to have urban residence, higher income, Hispanic ethnic identity, T2DM and obesity than patients in Groups 2 and 3 (all P<0.0001). Patients in Group 2 had significantly higher rates of T1DM, HTN, and HLD than patients in Groups 1 and 3 (all P<0.0001). Of non-fatal CVD admissions, 57% were for heart failure, 30% were for cerebrovascular events, and 13% were for acute coronary syndrome.
Anurag Goel,1 Joshua Tanzer2 & Vinit Gilvaz3
- The Warren Alpert Medical School of Brown University, Providence, R.I.
- Lifespan Biostatistics, Epidemiology, Research Design, and Informatics Core, Providence, R.I.
- The Warren Alpert Medical School of Brown University, East Providence, R.I.
Disclosures: A. Goel: None; J. Tanzer: None; V. Gilvaz: None
Citation
Goel A, Tanzer J, Gilvaz V. Psoriasis and psoriatic arthritis are independent risk factors for non-fatal cardiovascular admissions in transition-age young adults [abstract]. Arthritis Rheumatol. 2024;76(suppl 9).
Note: This research will be presented in a session at ACR Convergence 2024, Epidemiology & Public Health Poster I.


