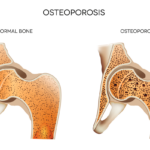
Patients with rheumatoid arthritis (RA) are at increased risk for the development of osteoporosis, due to inflammation-associated osteoclast activation and other reasons. Glucocorticoid use is also a well-established cause of osteoporosis, with osteoporotic fractures contributing to health-related costs and functional loss, morbidity and mortality for RA patients. To raise awareness to these concerns, the ACR published recommendations for the prevention and treatment of glucocorticoid-induced osteoporosis in 2010. The recommendations included calcium/vitamin D supplementation, use of a Fracture Risk Assessment Tool (FRAX) for all patients and bisphosphonate treatment for patients at a high risk for fracture.
Previous research noted a treatment gap, with only 30% of estimated eligible patients (65% of postmenopausal women and 52% of men age 50 years or older) receiving bisphosphonates. This treatment gap may also exist for RA patients for whom the need for osteoporosis screening and treatment interventions remains higher than the general population. Additionally, it is unknown if the 2010 ACR recommendations improved osteoporosis care of RA patients compared with patients at lower risk.
In a new study published in Arthritis Care & Research, May 2018, Gulsen Ozen, MD, of the University of Nebraska Medical Center, Omaha, and colleagues assessed the frequency, trends and predictors of osteoporosis treatment and screening in patients with RA compared with patients with osteoarthritis (OA). Researchers used data from the National Data Bank for Rheumatic Diseases for the longitudinal prospective observational study, with care defined as screening or receiving osteoporosis treatment (with the exception of calcium/vitamin D) or screening. The cohort consisted of 11,669 RA patients and 2,829 OA patients who received care and follow-up from 2003 through 2014.
The Results
“Approximately half of the RA patients were potential candidates for osteoporosis treatment by the 2010 ACR glucocorticoid-induced osteoporosis prevention [recommendations] or 2014 National Osteoporosis Foundation guideline. However, only approximately half of these patients ever received an osteoporosis medication,” write the authors.
Osteoporosis screening and treatment was reported in 67.4% of 11,669 RA patients and in 64.6% of 2,829 OA patients during a median of 5.5 (two to nine) years of follow-up. Of the patients for whom treatment was recommended, 48.4% of RA patients and 17.6% of OA patients reported osteoporosis medication use—approximately 55% overall. When compared with OA patients, RA patients were not more likely to undergo osteoporosis treatment or screening, after accounting for differences in socio-demographic features, BMI, glucocorticoid treatment, functional disability and FRAX 10-year major osteoporotic fracture risk categories.
In the study, the factors associated with receiving osteoporosis care in RA patients were being older or postmenopausal, having a prior fragility fracture or osteoporosis diagnosis, any duration of glucocorticoid treatment and use of biologic treatments.
Researchers conclude their paper by calling for research and clarification of patient- and provider-related factors for suboptimal management to develop effective interventions and reduce the burden of osteoporotic fractures on RA patients. “The development of an RA-specific osteoporosis prevention and management guideline may be helpful in covering all high-risk groups, optimizing osteoporosis care and decreasing the health impact of osteoporosis complications in RA,” they further conclude.
Ozen G, Kamen DL, Mikuls TR, et al. Trends and determinants of osteoporosis treatment and screening in patients with rheumatoid arthritis compared to osteoarthritis. Arthritis Care Res (Hoboken). 2018 May;70(5):713–723.